Research: Steven T. Haller, Ph.D.
 Associate Professor
Associate Professor
Director, Jacobson Center for Clinical and Translational Research
Research Coordinator and Project 4 Lead
Great Lakes Center for Fresh Waters and Human Health
Co-Director, Women & Philanthropy Genetic Analysis Center
Environmental, Occupational, and Community Medicine Program
Department of Medicine
Office: 419.383.6859
Laboratory: 419.383.6823
Fax: 419.383.6863
Email: Steven.Haller@UToledo.edu
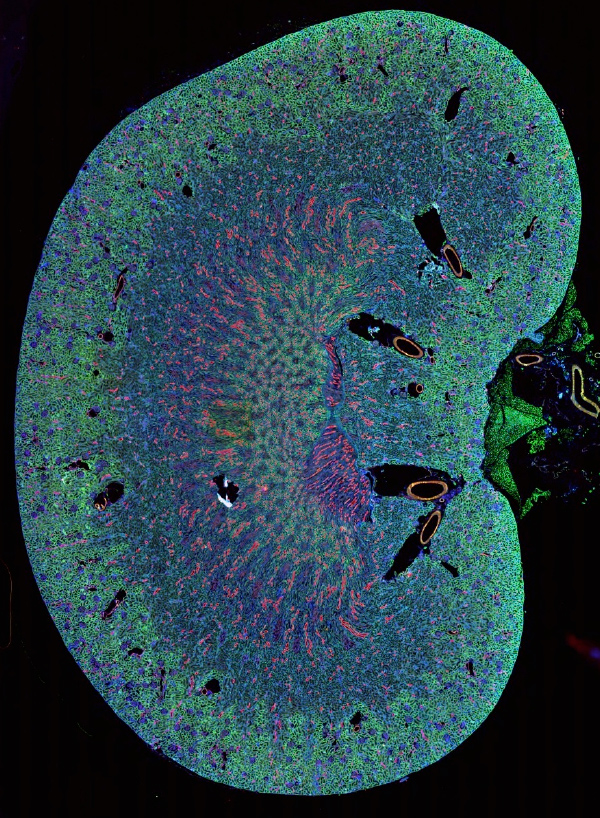
Lab Goal
The overall goal of my laboratory is to interrogate the molecular mechanisms leading to the development and progression of end stage renal disease. We are focusing our efforts on the mechanisms by which activation of the CD40 receptor within the kidney leads to progressive inflammation and fibrosis with the ultimate goal of providing a therapeutic approach to inhibit the development of end stage renal disease. In addition to investigating the molecular mechanisms leading to end stage renal disease, my lab is also focused on the health effects of cyanotoxin exposure in pre-existing disease states. Importantly, as harmful algal blooms are on the rise globally and across the state of Ohio, the cyanotoxins they generate pose potentially serious health concerns to humans and animals, especially in vulnerable at-risk populations.
Education
B.S., Biology/Chemistry, University of Toledo, 2003
M.S., Molecular Basis of Disease, Medical University of Ohio, 2005
Ph.D., Biomedical Sciences, University of Toledo Health Science Campus, 2012
Postgraduate Training
- University of Toledo Health Science Campus, Department of Medicine, 2012-2015
- American Heart Association Postdoctoral Fellowship, 2013-2015
Academic Appointments
- Associate Professor of Medicine, Division of Cardiovascular Medicine, Department of Medicine, University of Toledo College of Medicine and Life Sciences
- Joint Appointment: Department of Medical Education, University of Toledo College of Medicine and Life Sciences
Awards and Commendations
- American Heart Association Postdoctoral Fellowship, 2013-2015
- European Society of Hypertension and International Society of Hypertension Travel Award, 2014
- European Society of Hypertension and International Society of Hypertension Finalist for Young Investigator Award, 2014
Research Interests:
Molecular Mechanisms Leading to End Stage Renal Disease
 Hypertension leading to the development of end-stage renal disease (hypertensive nephropathy)
is common, prevalent in up to 30% of patients in the United States, and currently
the second leading cause of end-stage renal disease despite treatment strategies aimed
at blood pressure control and the use of renin-angiotensin inhibitors. Renal inflammation
has been implicated in the progression of hypertensive nephropathy. However, the exact
mechanisms and therapeutic approaches remain to be elucidated.
Hypertension leading to the development of end-stage renal disease (hypertensive nephropathy)
is common, prevalent in up to 30% of patients in the United States, and currently
the second leading cause of end-stage renal disease despite treatment strategies aimed
at blood pressure control and the use of renin-angiotensin inhibitors. Renal inflammation
has been implicated in the progression of hypertensive nephropathy. However, the exact
mechanisms and therapeutic approaches remain to be elucidated.
Our work suggests that activation of the CD40 receptor (a TNF-receptor superfamily costimulatory molecule) plays a crucial role in the development of hypertensive nephropathy and represents a potential treatment strategy to inhibit renal inflammation and renal fibrosis. Soluble CD40 ligand (sCD40L) is expressed and secreted by activated platelets and is an important mediator of immunity, inflammation, and coagulation. In proximal tubular epithelial cells, sCD40L signaling through the CD40 receptor activates pro-inflammatory and pro-fibrotic signaling cascades.
We have recently shown that circulating levels of CD40 predict progression of renal dysfunction in patients with ischemic and chronic kidney disease (CKD) and that sCD40L is significantly elevated in these settings. To transition our clinical findings to an experimental model, we have recently created a novel Cd40 mutant rat on a genetic background prone to the development of hypertensive renal injury (Dahl S strain). Using these Cd40 mutant rats in which CD40 signaling is abolished, we have demonstrated markedly reduced renal fibrosis and improved renal function vs. the wild type control Dahl S rats. In addition, we are investigating a novel regulatory mechanism by which cardiotonic steroid signaling activates CD40 in the proximal tubule epithelium. We are also developing novel peptide inhibitors of CD40 signaling as a potential therapeutic approach.
Effects of Cyanotoxin Exposure in Pre-existing Disease States
Our lab is an active member of the University of Toledo Water Task Force with the central mission to investigate the potentially harmful effects of algal blooms on the surrounding community. Algal blooms cause drastic increases in the release of cyanotoxins produced by cyanobacteria, which can contaminate freshwater sources and pose serious health risks to humans. Importantly, these blooms occur frequently not only in every single region of the US, but have been reported with increased frequency in almost every country world-wide. The health based criteria for safe exposure limits to cyanotoxins has been extrapolated to humans from toxicology studies performed only in healthy animal models and the effect of these toxins in the setting of at-risk populations, such as those with pre-existing disease states, is unknown. To bridge this important knowledge gap, we are investigating the effects of cyanotoxin exposure in models of pre-existing disease to determine if cyanotoxin exposure exacerbates disease progression and to develop diagnostic tests of exposure.

Photo of Lake Erie algal bloom courtesy Cruising Odyssey
Media
Publications
Haller ST, Kumarasamy S, Folt DA, Wuescher LM, Stepkowski S, Karamchandani M, Waghulde H, Mell B, Chaudhry M, Maxwell K, Upadhyaya S, Drummond CA, Tian J, Filipiak WE, Saunders TL, Shapiro JI, Joe B, Cooper CJ. Targeted disruption of Cd40 in a genetically hypertensive rat model attenuates renal fibrosis and proteinuria, independent of blood pressure. Kidney Int. 2017;91:365-374.
Xie XJ, Alderson H, Ritchie J, Kalra PA, Xie Y, Ren K, Nguyen H, Tian C, Brewster P, Gupta R, Dworkin LD, Malhotra D, Cooper CJ, Tian J, Haller ST. Circulating CD40 and sCD40L predict changes in renal function in subjects with chronic kidney disease. Scientific Reports. 2017:7;7942.
Xie JX, Fan X, Drummond CA, Majumder R, Xie Y, Chen T, Liu L, Haller ST, Brewster PS, Dworkin LA, Cooper CJ, Tian J. MicroRNA profiling in kidney disease: Plasma verses plasma-derived exosomes. Gene. 2017;627:1-8.
Drummond, CA, Brewster PS, He W, Ren K, Xie Y, Tuttle KA, Haller ST, Jamerson K, Dworkin LD, Cutlip DE, Murphy TP, D’Agostino RB, Henrich WL, Tian J, Cooper CJ. Cigarette Smoking and Cardio-Renal Events in Patients with Atherosclerotic Renal Artery Stenosis. 2017 PloS one. 2017;12(3):e0173562.
Haller ST, Yan Y, Drummond CA, Xie J, Tian J, Kennedy DJ, Shilova VY, Xie Z, Liu J, Cooper CJ, Malhotra D, Shapiro JI, Fedorova OV, Bagrov AY. Rapamycin Attenuates Cardiac Fibrosis in Experimental Uremic Cardiomyopathy by Reducing Marinobufagenin Levels and Inhibiting Downstream Pro-Fibrotic Signaling. J Am Heart Assoc. 2016 Sep 30;5(10). pii: e004106. PubMed PMID: 27694325.
Liu J, Tian J, Chaudhry M, Maxwell K, Yan Y, Wang X, Shah PT, Khawaja AA, Martin R, Robinette TJ, El-Hamdani A, Dodrill MW, Sodhi K, Drummond CA, Haller ST, Kennedy DJ, Abraham NG, Xie Z, Shapiro JI. Attenuation of Na/K-ATPase Mediated Oxidant Amplification with pNaKtide Ameliorates Experimental Uremic Cardiomyopathy. Sci Rep. 2016 Oct 4;6:34592. doi: 10.1038/srep34592. PubMed PMID: 27698370.
Drummond CA, Crotty Alexander LE, Haller ST, Fan X, Xie JX, Kennedy DJ, Liu J, Yan Y, Hernandez DA, Mathew DP, Cooper CJ, Shapiro JI, Tian J. Cigarette Smoking Causes Epigenetic Changes Associated With Cardiorenal Fibrosis. Physiol Genomics. 2016;48:950-960.
Yan Y, Shapiro AP, Mopidevi BR, Chaudhry MA, Maxwell K, Haller ST, Drummond CA, Kennedy DJ, Tian J, Malhotra D, Xie ZJ, Shapiro JI, Liu J. Protein Carbonylation of an Amino Acid Residue of the Na/K-ATPase α1 Subunit Determines Na/K-ATPase Signaling and Sodium Transport in Renal Proximal Tubular Cells. J Am Heart Assoc. 2016 Sep 9;5(9). pii: e003675. doi: 10.1161/JAHA.116.003675. PubMed PMID: 27613772.
Shi H, Drummond CA, Fan X, Haller ST, Liu J, Malhotra D, Tian J. Hiding inside? Intracellular expression on non-glycosylated c-kit protein in cardiac progenitor cells. Stem Cell Res. 2016;16:795-806.
Ren K, Drummond D, Brewster PS, Haller ST, Tian J, Cooper CJ, Zhang B. An alternative empirical likelihood method in missing response problems and causal inference. Stat Med. 2016;35:5009-5028.
Drummond CA, Hill MC, Shi H, Fan X, Xie JX, Haller ST, Kennedy DJ, Liu J, Garrett MR, Xie Z, Cooper CJ, Shapiro JI, Tian J. Na/K-ATPase signaling regulates collagen synthesis through microRNA-29b-3p in cardiac fibroblasts. Physiol Genomics. 2016;48:220-9.
Folt DA, Evans KL, Brahmandam S, He W, Brewster PS, Yu S, Murphy TP, Cutlip DE, Dworkin LD, Jamerson K, Henrich W, Kalra PA, Tobe S, Thomson K, Holden A, Rayner BL, Grinfeld L, Haller ST, Cooper CJ. Regional and physician specialty-associate variations in the medical management of atherosclerotic renal-artery stenosis. J Am Soc Hypertens. 2015;9:443-52.
Haller ST, Drummond CA, Yan Y, Liu J, Tian J, Malhotra D, Shapiro JI. Passive immunization against marinobufagenin attenuates renal fibrosis and improves renal function in experimental renal disease. AM J Hypertension. 2014;27:603-609.
Sayed M, Drummond CA, Evans KL, Haller ST, Liu J, Xie Z, Tain J. Effects of Na/K-ATPase and its ligands on bone marrow stromal cell differentiation. Stem Cell Res. 2014;13:12-23.
Yu MS, Folt DA, Drummond CA, Haller ST, Cooper EL, Brewster P, Evans KL, Cooper CJ. Endovascular verses medical therapy for atherosclerotic renovascular disease. Curr Atheroscler Rep. 2014;16:459
Evans KL, Tuttle KR, Folt DA, Dawson T, Haller ST, Brewster PS, He W, Jamerson K, Dworkin LD, Cutlip DE, Murphy TP, D’Agostino RB Sr, Henrich W, Cooper CJ. Use of renin-angiotensin inhibitors in people with renal artery stenosis. Clin J AM Soc Nephrol. 2014;9:1199-206.
Drummond CA, Sayed M, Evans KL, Shi H, Wang X, Haller ST, Liu J, Cooper CJ, Xie Z, Shapiro JI, Tian J. Reduction of Na/K-ATPase affects cardiac remodeling and increases c-kit cell abundance in partial nephrectomized mice. Am J Physiol Heart Circ Physiol. 2014 Jun 15;306(12):H1631-43. doi: 10.1152/ajpheart.00102.2014. Epub 2014 Apr 18. PubMed PMID: 24748592; PubMed Central PMCID: PMC4059984.
Haller ST, Evans KL, Folt DA, Drummond CA, Cooper CJ. Mechanisms and treatments for renal artery stenosis. Discov Med. 2013;16:255-260.
Haller ST, Kalra PA, Ritchie JP, Chrysochou T, Brewster P, He W, Yu H, Shapiro JI, Cooper CJ. Effect of CD40 and sCD40L on Renal Function and Survival in Patients with Renal Artery Stenosis. Hypertension. 2013;61:894-900.
Fedorova LV, Tamirisa A, Kennedy DJ, Haller ST, Budny G, Shapiro JI, Malhotra D. Mitochondrial impairment in the fifth-sixth nephrectomy model of chronic renal failure: proteomic approach. BMC Nephrol. 2013;4:209.
Drummond CA, Buddny G, Haller ST, Liu J, Yan Y, Xie Z, Malhotra D, Shapiro JI, Tian J. Gender differences in the development of uremic cardiomyopathy following partial nephrectomy: Role of progesterone. J Hypertens (Los Angel). 2013 Jan 31;2. doi: 10.4172/2167-1095.1000109. PubMed PMID: 24404431; PubMed Central PMCID: PMC3880896.
Yan Y, Shapiro AS, Haller S, Katragadda V, Liu L, Tian J, Basrur V, Malhotra D, Xie ZJ, Abraham NG, Shapiro JI, Liu J.Involvement of reactive oxygen species in a feed-forward mechanism of Na/K-ATPase-mediated signal transduction. J Biological Chem. 2013;288:34249-34258.
Haller S, Kennedy DJ, Shidyak A, Budny G, Malhotra D, Fedorova OV, Shapiro JI, Bagrov AY. Monoclonal antibody against marinobufagenin reverses cardiac fibrosis in rats with chronic renal failure. Am J Hypertension. 2012;25:690-6.
Yan Y, Haller S, Shapiro A, Malhotra N, Tian J, Xie Z, Malhotra D, Shapiro, JI, Liu J. Ouabain-stimulated trafficking regulation of the Na/K-ATPase and NHE3 in renal proximal tubule cells. Mol Cell Biochem, 2012;367:175-183.
Haller S, Adlakha S, Reed G, Brewster P, Kennedy D, Burket MW, Colyer W, Yu H, Zhang D, Shapiro JI, Cooper CJ. Platelet activation in patients with atherosclerotic renal artery stenosis undergoing stent revascularization. Clin J Am Soc Nephrol. 2011;6:2185-91.
Yu H, Zhang D, Haller S, Kanjwal K, Colyer W, Brewster P, Steffes M, Shapiro JI, Cooper CJ. Determinants of renal function in patients with renal artery stenosis. Vasc Med. 2011;16:331-8.
Kolmakova EV, Haller ST, Kennedy DJ, Isachkina AN, Budny GV, Frolova EV, Piecha G, Nikitina ER, Malhotra D, Fedorova OV, Shapiro JI, Bagrov AY. Endogenous cardiotonic steroids in chronic renal failure. Nephrol Dial Transplant. 2011;26:2912-9.
Tian J, Haller S, Periyasamy S, Brewster P, Zhang H, Adlakha S, Fedorova OV, Xie ZJ, Bagrov AY, Shapiro JI, Cooper CJ. Renal ischemia regulates marinobufagenin release in humans. Hypertension. 2010;56:914-9.
Kanjwal K, Cooper CJ, Virmani R, Haller S, Shapiro JI, Burket MW, Steffes M, Brewster P, Zhang H, Colyer WR Jr. (2010) Predictors of embolization during protected renal artery angioplasty and stenting: Role of antiplatelet therapy. Catheter Cardiovasc Interv. 2010;76:16-23.
Tian J, Shidyak A, Periyasamy SM, Haller S, Taleb M, El-Okdi N, Elkareh J, Gupta S, Gohara S, Fedorova OV, Cooper CJ, Xie Z, Malhotra D, Bagrov AY, Shapiro JI. Spironolactone attenuates experimental uremic cardiomyopathy by antagonizing marinobufagenin. Hypertension. 2009;54:1313-20.
Kanjwal K, Haller S, Steffes M, Virmani R, Shapiro JI, Burket MW, Cooper CJ, Colyer WR Jr. (2009) Complete versus partial distal embolic protection during renal artery stenting. Catheter Cardiovasc Interv, 2009;73:725-30.
Cooper CJ, Haller ST, Colyer W, Steffes M, Burket MW, Thomas WJ, Safian R, Reddy B, Brewster P, Ankenbrandt MA, Virmani R, Dippel E, Rocha-Singh K, Murphy TP, Kennedy DJ, Shapiro JI, D'Agostino RD, Pencina MJ, Khuder S. (2008) Embolic protection and platelet inhibition during renal artery stenting. Circulation, 2008;117:2752-60.
Dr. Haller discloses funding from Abbott, Inc. and attests that:
a) these funds are not sole clinical or educational resources or a source to learners
b) this relationship/affiliation will not bias or otherwise influence Dr. Kennedy's
involvement in any CME activity
c) practice recommendations given relevant to the companies with whom I have relationships/affiliations
will be supported by best available evidence or, absent evidence, will be consistent
with generally accepted medical and scientific practice and
d) that all reasonable clinical alternatives will be discussed when making practice
recommendations.


