Resident and Faculty Evaluation
The RRC mandates that all residents be provided with feedback on progress at the mid-point of each rotation (formative feedback). The residency office can provide you with the template. If there is more than one faculty member on the rotation, this can be designated to one person, who can share the insights of the group. This feedback should focus on areas of strength and areas of improvement to that point. This is particularly critical if the resident is in jeopardy of not passing the rotation. This feedback does not need to be documented, but it must be given.
End of month feedback is provided by the global evaluation (summative) new innovations, you provide at the end of the rotation. These are described below under "evaluation". Faculty is encouraged to go over the evaluation at the end of the month.
EVALUATIONS:
-
Evaluations must be submitted in a timely manner. Ideally, they should be done within one week. Delayed evaluation prevents residents from receiving needed feedback and prevents the program from conducting formal semi-annual evaluations.
-
All faculty should evaluate, regardless of the extent of contact. For example, if you only spend two half days with the resident, please still evaluate based on that degree of contact. If multiple faculty participate on your rotation, the group may wish to meet and fill out one overall evaluation. Some may worry that they are "Certifying" competency for a resident's future performance, based on a limited amount of contact. This is one worry you can let go. You are only making an assessment based on the degree of contact. For example, let's assume you worked with a resident for two half-day sessions. If you mark "competent" on history taking, you are not indicating that the resident is automatically able, then and there, to take histories on any patient without supervision. You are only commenting on how they did for the level of contact you had. The program and program director is responsible, in the end, for signing off that residents and graduates are competent to practice without supervision.
-
Please provide specific comments within the evaluation where indicated. Residents have found specific comments to be the most useful in improving future performance.
-
Residents and faculty evaluate each other through the New Innovations system
-
How to access new innovations:
Goto www.new-innov.com/Login/Login.aspx
Please contact Tiffany Lopez if you do not know your Institution Login, Username, or Password at tiffany.lopez@utoledo.edu or by phone at (419) 383-6821.
You are expected to review your evaluations by the residents and accept them on new innovations.
PGY 1 resident must not be assigned more than five new patients per admitting day, additional 2 in house transfer patients from medical services may be assigned. PGY 1 resident must not be assigned more than eight new patients in a 48 hour period. PGY 1 resident must not be responsible for the ongoing care of more than 10 patients.
Resident supervising more than one PGY 1 resident must not be responsible for the supervision or admission of more than 10 new patients per admitting day or more than 16 new patients in 48 hour period. Resident supervising one PGYI resident must not be responsible for ongoing care of more than 14 patients. Resident supervising more than one PGY 1 must not be responsible for ongoing care of more than 20 patients.
Residents must write all orders for patient under their care, with supervision by the attending physician. Attending physician or subspecialty resident writing an order on a residents' patient must communicate the action to the resident.
AMBULATORY ROTATION
At least 1/3 of resident's time should be spent in ambulatory training.
What counts as ambulatory training?
Outpatient subspecialty, GIM Longitudinal Clinic, Ambulatory rotation and the VA clinic.
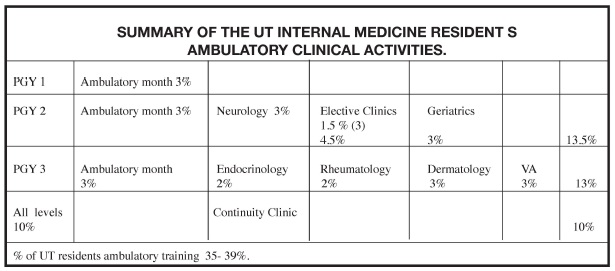
CONTINUITY CLINIC
- Has to have 133 clinics in 3 years effective July 2009 –prior residents are grandfathered to 108 clinics.
- Data driven feedback
- RRC demands we give residents data driven feedback on patient care - ABIM practice improvement module
- Utilizing admitting residents 'scholarly activity' time
- EMR will ease this burden
UT Internal Medicine experience in measuring the Six Competencies.
"Whatever we measure, we tend to improve"
"These competencies and attempts to assess them contribute to the medical professions attempt to regulate itself”.
"Competence develops over time and is nurtured by reflection on experiences"
– Dr. David Leach
"To become competent you must feel bad"
– Hubert Dreyfus
Measuring the competencies involves collecting all the activities that represents the 1) resident's efforts, 2) progress and the 3) achievements in multiple areas of the curriculum.
Advantages:
1)To better understand how to integrate the competencies into education.
2)Mold the education of the six competencies to a more instructive task.
3)Assessment results can provide formative and summative feedback to residents.
The score card was reviewed with the residents and with the faculty. We started to implement it in January 2010.
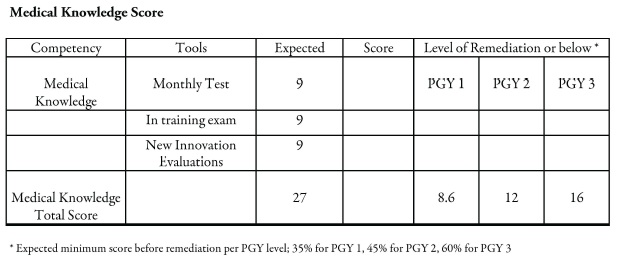
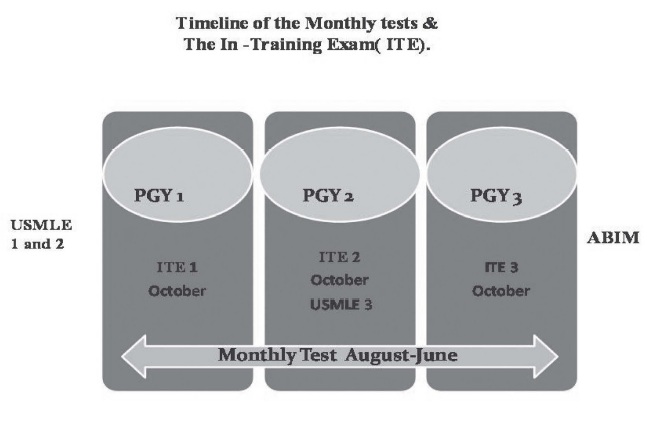
Medical Knowledge:
We use the following tools to quantify medical knowledge:
1)Monthly test.
2)National In-Training Exam.
3)New Innovations (Global Assessment) / Faculty assessment.