COVID-19 Situational Updates for HSC
Page updated: May 27, 2022, 3 p.m. Vaccine Requirement
 UTMC Hospital and Clinics are required to wear a disposable, hospital-grade mask while
in patient care areas. It is also required for visitors to wear a mask while they
are at the healthcare facility.
UTMC Hospital and Clinics are required to wear a disposable, hospital-grade mask while
in patient care areas. It is also required for visitors to wear a mask while they
are at the healthcare facility.
This webpage provides you with up-to-date information to help protect you, and help you do your job.
Sections on page: Top Topics (see tabs below) | Hotlines | Best Way to Prevent Illness | Ambulatory | UTMC | Newsletter Archive
COVID-19 At-A-Glance | News | Clinical Trials | Updates from the Governor | Data Sources
- UTMC Numbers / Testing
- Return to Work Protocol
- Restart
- PPE
- Diagnosis / Treatment
- Patients
- Discharge Info
- Clinical Features
- Staying Well
- Incident Command
- Questions
Section Last Updated: May 18, 2022, 5 p.m.
UTMC COVID-19 Cases Update (May 18)
On March 24, 2020, we had our first confirmed case of COVID-19 at UTMC.
Below, find a table of our current numbers:
| Tested | Confirmed Currently Hospitalized |
||||||||||||||||
| Total number of positive cases UTMC has tested: Total positive: 4,520 (+32 since May 12) (includes outpatient and |
|
COVID-19 Testing (Jan. 5, 2022)
UTMC COVID testing has expanded available testing:
SYMPTOMATIC TESTING:
Covid-19 Testing (Expanded Hours Monday – Friday 9am-5pm)
We have updated the COVID-19 testing line 419.383.4545 to include more options to better serve you. When the following numbers are selected you will be directed to the following:
- Option 1: Health Science Campus SYMPOMATIC Testing – Forwarded to voicemail for COVID-19 testing. Your call will be returned within 24 hours Monday through Friday. If you call over the weekend, your call will be returned on Monday. The testing center is now located at the Glendale Medical Center, 3333 Glendale Avenue.
- Option 2: Main Campus Testing (UToledo students, faculty, and staff only) – Forwarded to University Health Center on Main Campus voicemail for COVID-19 testing.
Your call will be returned within 24 hours.
- Testing at this location is only for Symptomatic Students, Faculty and Staff of the University, UTMC, and UTP as well as any family members in the household that has been exposed or anyone with a positive rapid test that comes from your team. There is no testing for the public at this location and they are not instructing the public to any of UT’s other testing sites.
- Option 3: Vaccines – Forwarded to OP Pharmacy.
- Option 4: Monoclonal antibodies – Forwarded to 419.383.4432. Your call will be returned the same business day to schedule the patient’s treatment.
ASYMPTOMATIC TESTING:
Employees, faculty and staff that have not been vaccinated are required to have weekly COVID testing. They may schedule a test online by using this link: covid19test.utoledo.edu
This clinic is for asymptomatic people only. If you become symptomatic prior to your scheduled test, please cancel and call 419-383-4545 to schedule a PCR test.
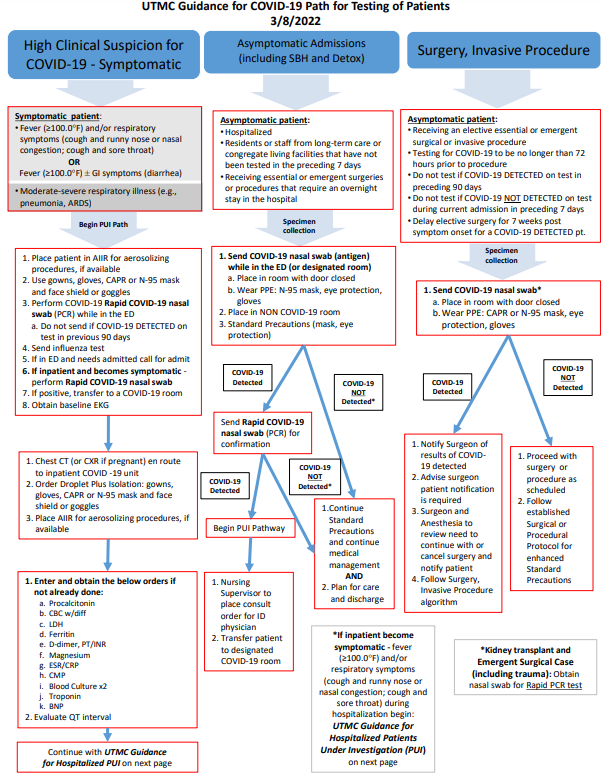
Testing Algorithm Update for COVID-19 (March 14, 2022)
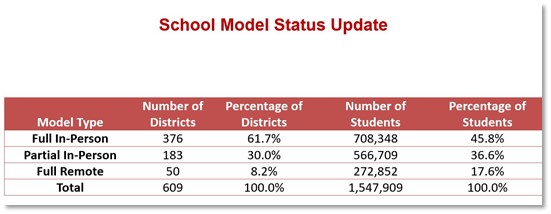
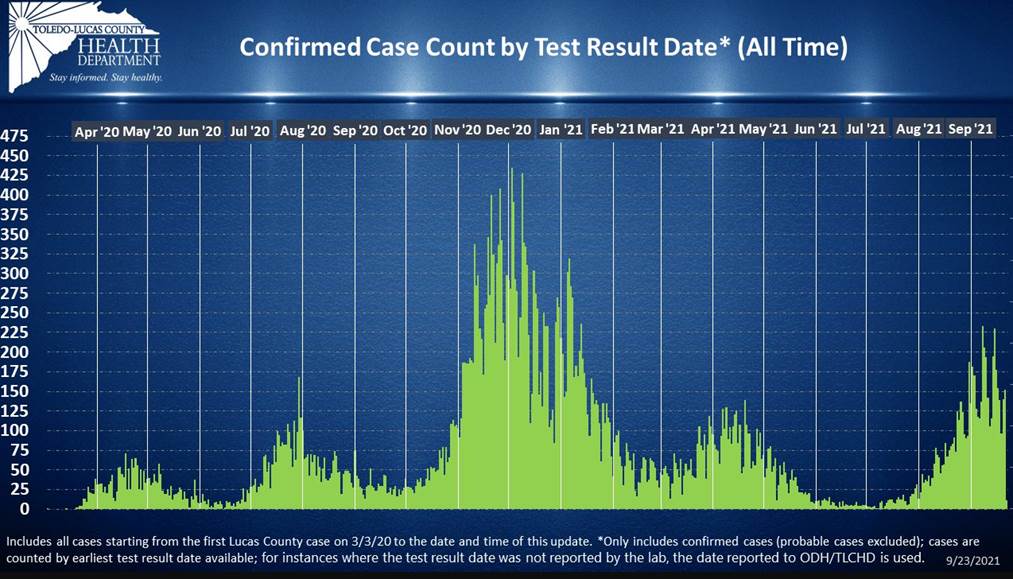
Lucas County Cumulative Daily Data And Trends (Sept. 24)
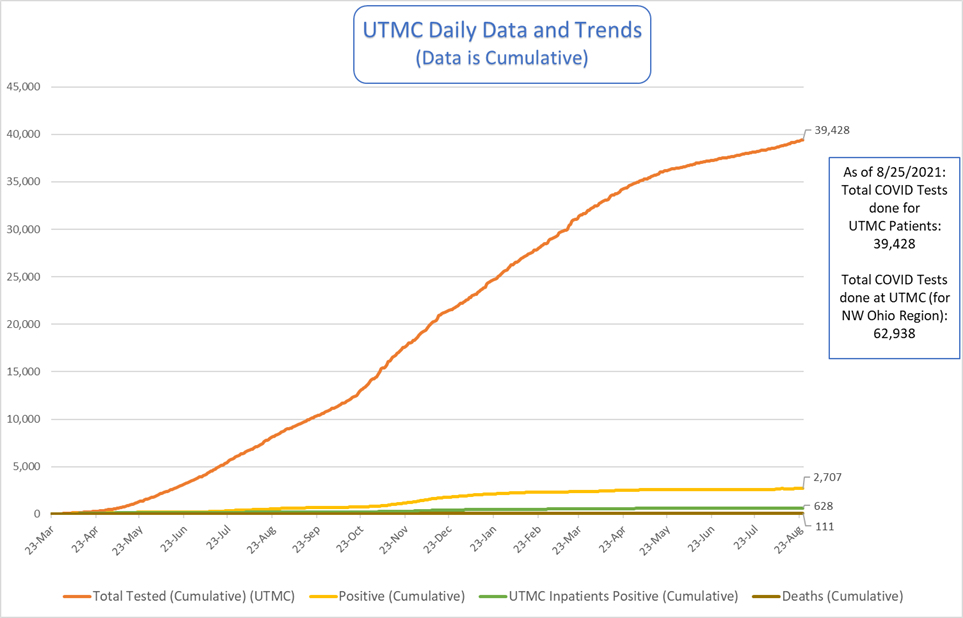
UTMC Cumulative Daily Data and Trends (Aug. 27)
Transmission Rate (Aug. 11)
Lucas County community transmission rate at 84.5 per 100,000 population, which has increased from previous weeks. Lucas County is at 74 out of 88 counties as it pertains to cases per 100,000 (highest being Scioto county with a rate of 397.0 per 100,000 population and the lowest being Holmes county with a rate of 34.1 per 100,000 population).
Testing
The Ohio Department of Health Lab is performing Whole Genome Sequencing (WGS) on vaccine breakthrough cases as well as through passive surveillance. The goal is to identify Variants of Concern (VOC) in Ohio residents. The Toledo-Lucas County Health Department has been notified of several cases of VOC identified in Lucas County residents. Currently, all cases identified have been through passive surveillance. We are attempting to send every vaccine breakthrough case we're notified of.
Learn more about testing in Ohio
Variant Proportions
CDC's national genomic surveillance program identifies new and emerging SARS-CoV-2
variants to determine implications for COVID-19 diagnostics, treatments, or vaccines
authorized for use in the United States. Monitoring the spread of emerging variants
in the United States relies on widespread, rapid sequencing. To accelerate sequencing
in the United States, CDC has contracted with commercial diagnostic laboratories,
and, in partnership with the Association of Public Health Laboratories (APHL), has
implemented the National SARS-CoV-2 Strain Surveillance (NS3) program to provide a
comprehensive and population-based US surveillance system.
Based on these data, sequences with similar genetic changes associated with important
epidemiological and biological events are grouped into lineages. A viral lineage is
a group of viruses defined by a founding variant and its descendants. The proportion
of lineages circulating in the United Stated are tracked and characterized to determine
if they are considered variants of concern (VOC) or variants of interest (VOI). Most
of the lineages identified through genomic surveillance do not fall into either of
these categories. These data, along with data from many other sources, are used to
inform national and state public health actions related to variants.
COVID-19 screening tool
Download the COVID-19 Screening Tool.
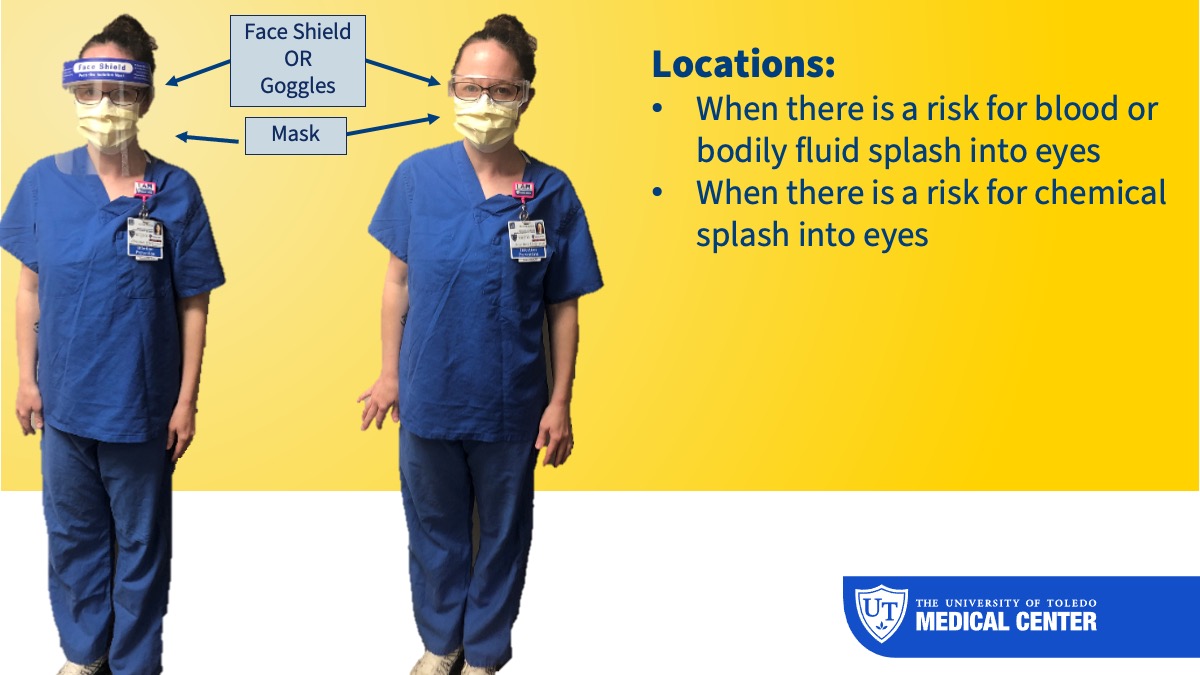
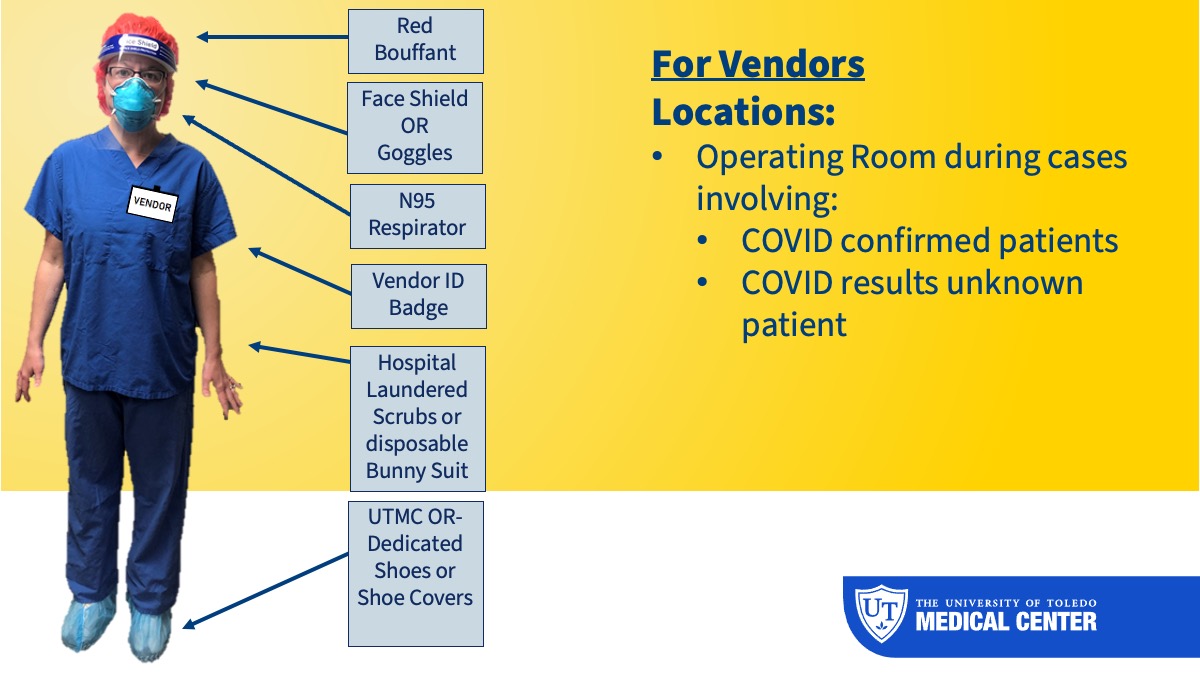
Reminder: The identification of Aerosol-Generating Procedures (Feb. 4)
PRIOR to performing aerosol generating procedures on COVID-19 suspected or confirmed patients, you must obtain the following supplies:
- N-95 mask or CAPR if not fit testing or with facial hair
- Goggles/Face shield (with N-95 use)
- Gown
- Gloves
Updated education for COVID-19 testing (Oct. 9)
Video: Collecting swab specimens (June 1)
Watch video for collecting oral pharyngeal and nasal pharyngeal swab specimens to test for COVID-19. Before obtaining the sample, please make sure that you are aware of the route for which to obtain the sample and that you are educating your patient on the process.
Section Last Updated: Jan. 25, 2022, 3 p.m.
Return To Work Criteria
Return to Work Criteria For UToledo Employees (Jan. 5, 2022)
Updates to this document:
- 10 days return changed to 5 day return if without a fever and if symptoms have improved
- Definition of fully vaccination changed to: Are boosted -OR- Have completed the primary series of Pfizer or Moderna vaccine within the last 6 months -OR- Received one dose of J&J vaccine within the last 2 months:
- Return to Work Practices and Work Restrictions updated for both Healthcare Providers and Non-Healthcare Providers
Updates to process: Occupational Health/COVID Testing Clinic will be assisting employees, faculty and
staff tested through the COVID Testing Clinic at UTMC with their return to work information
effective January 18, 2022.
Infection Prevention will continue to provide COVID resources for employees, faculty
and staff tested at facilities other than the UTMC COVID Testing Clinic and they will
continue to be available to answer questions or concerns from employees, as needed.
Section Last Updated: Aug. 17, 2021, 2 p.m.
Temporary Visitor Restrictions at UTMC (Aug. 17, 2021)
Effective immediately, we are decreasing the number of visitors allowed from two to one in several areas.
Please see the most up-to-date visitor information here or below:
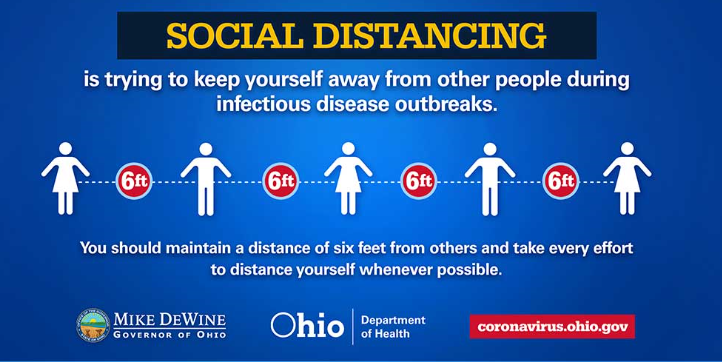
Visitors must wear a mask that covers nose and mouth at all times.
Maintain 6 Feet social distancing in all waiting rooms.
Visitors are welcome from 11 a.m. to 8:30 p.m. with exceptions noted below.
Visitors must be 16 years of age or have special permission from Nursing Director, and/or their designee (House Supervisor/ Charge Nurse).
Off hour visitation is only available with special permission from Nursing Director, and/or their designee (House Supervisor/ Charge Nurse). Limit of one visitor per patient during off hour visitation.
Inpatient Units (Non-COVID)
Limited to one visitor per patient at one time
End of Life/Hospice (Non-COVID)
Up to four visitors at same time are allowed at bedside without restriction to time of day, as approved by staff.
Medical Intensive Care Unit (MICU)
Immediate family only. Limited to one visitor per patient at one time.
COVID Unit
No visitors unless medically necessary for the care of the patient and/or for special circumstances. (Visitor's must wear all PPE, including a mask that covers nose and mouth at all times)
These special circumstances include:
- At end of life, up to two visitors are allowed at the bedside without restrictions on time of day, as approved by staff.
- Religious services from clergy of their choice, during visitation hours, without disruption of their care.
- End of life religious services are permitted.
- Patients with disabilities may have two designated support persons or guardians stay with them. One may remain overnight if hospital can accommodate them.
Emergency Department
Limit of one visitor per patient at a time. 16 years of age or older. Visitor must
remain at bedside.
(2 visitors for minor child).
Surgery and Procedural Areas
Inpatient: Limit of one visitor, 16 years of age or older. Must remain in designated waiting
area.
Outpatient: Limit of one visitor/ driver, 18 years of age or older. Must remain in designated
waiting area.
Ambulatory Clinics
Limit of one visitor, 16 years of age or older. Must remain with the patient at all times.
Infusion Centers and Radiation Oncology
No visitors unless medically necessary for the care of the patient and/or for special circumstances. (Visitor's must wear all PPE, including a mask that covers nose and mouth at all times).
These special circumstances include:
- Religious services from clergy of their choice, without disruption of their care.
- Patients with disabilities may have two designated support persons or guardians stay with them.
COVID-19 positive/High Clinical Suspicion admissions at UTMC (Effective June 8, 2021)
- Admissions:
- Will go to a negative pressure room (if available) on the appropriate unit/level of care.
- Follow all isolation procedures for COVID-19.
- Use proper donning/Doffing, N95 masks, Eye protection
- Nurse assigned can care for normal assignment.
- Manage assignments to avoid caregiver from caring for another immune compromised patient (e.g., chemo)
- Minimize number of staff caring for patient in isolation
- Ensure assigned nurse was mask fit tested and had COVID-19 PPE training
- Opening the Surge COVID Unit, at the discretion of the CNO/ House Supervisors.
- Reasons:
- Unable to admit COVID-19 patients due to lack of available negative pressure rooms
- Surge of COVID-19 positive patients in our community requiring hospitalization
- Reasons:
FEMA Advisory (April 2)
FEMA will be providing financial assistance (reimbursement) for funeral expenses incurred after January 20, 2020, specifically for COVID-19 deaths. Additional information is attached. Individuals will apply directly to FEMA.
Johnson & Johnson’s Janssen COVID-19 Vaccine
UTMC’s Antimicrobial Stewardship Pharmacist provided information about the efficacy of the Johnson & Johnson vaccine.
Travel advisories
Complete CDC guidance on travel can be found here: Domestic Travel During the COVID-19 Pandemic
Screening updates (Feb. 26)
The hospital proper continues to have greeters at the main entrance and medical pavilion to manage the visitors. Visitors will be screened upon entry per CDC recommendations updated on Feb. 22. We will continue with current visitation policy.
The CDC still encourages:
- Establish a process to ensure everyone (patients, healthcare personnel, and visitors) entering the facility is assessed for symptoms of COVID-19, or exposure to others with suspected or confirmed SARS-CoV-2 infection and that they are practicing source control.
- Options could include (but are not limited to): individual screening on arrival at the facility; or implementing an electronic monitoring system in which, prior to arrival at the facility, people report absence of fever and symptoms of COVID-19, absence of a diagnosis of SARS-CoV-2 infection in the prior 10 days, and confirm they have not been exposed to others with SARS-CoV-2 infection during the prior 14 days.
guidelines approved for pregnant employees
At UTMC, pregnant individuals will not be providing care to known COVID-19 positive patients. See link to the updated guidelines for pregnant healthcare workers below.
Based on what is known at this time, pregnant women are at an increased risk for severe illness from COVID-19 compared to non-pregnant women. Additionally, pregnant women with COVID-19 might have an increased risk of adverse pregnancy outcomes, such as preterm birth. Read more on the CDC website about investigating the impact of COVID-19 during pregnancy.
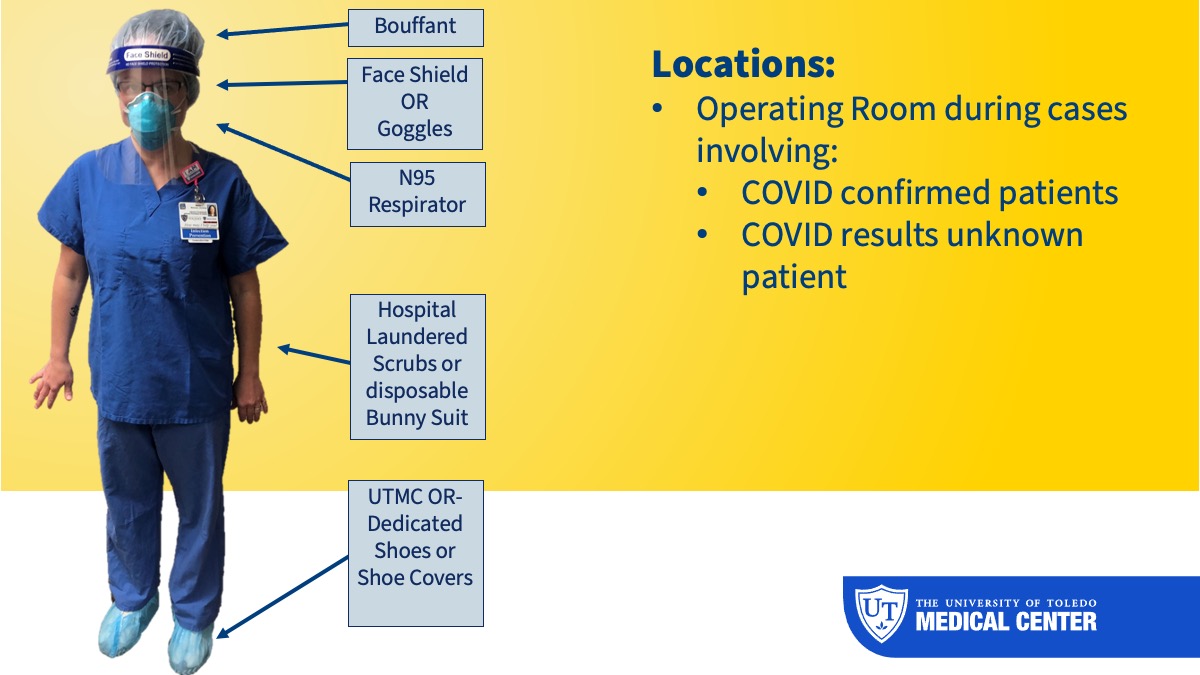
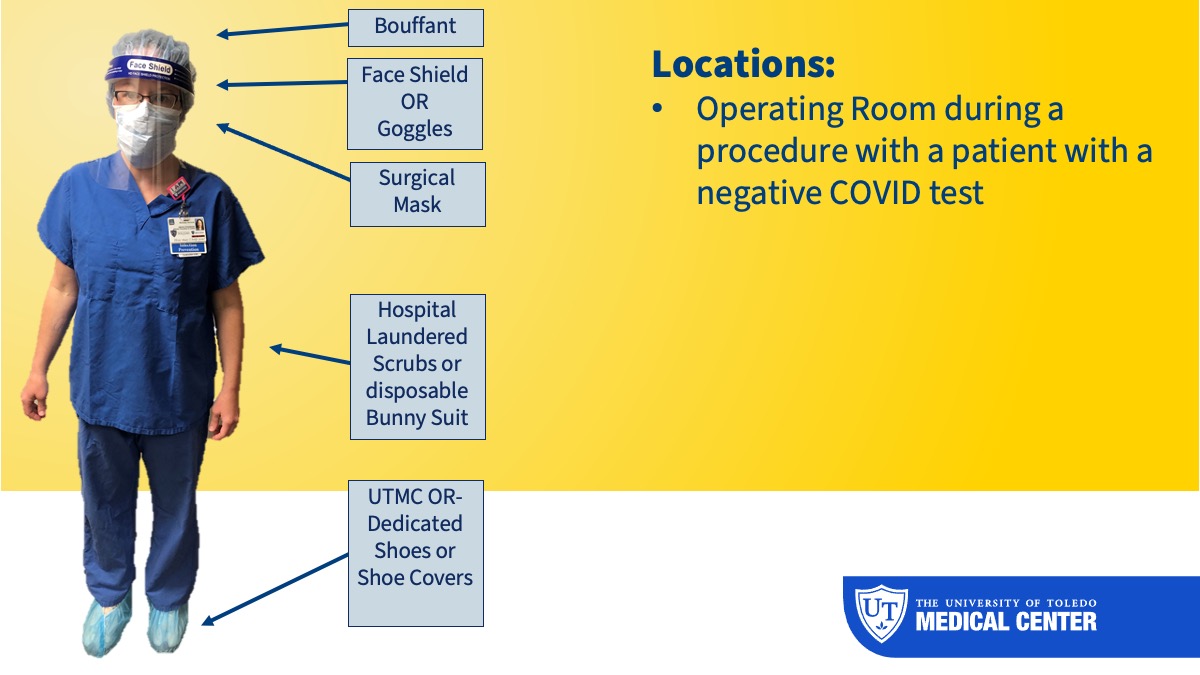
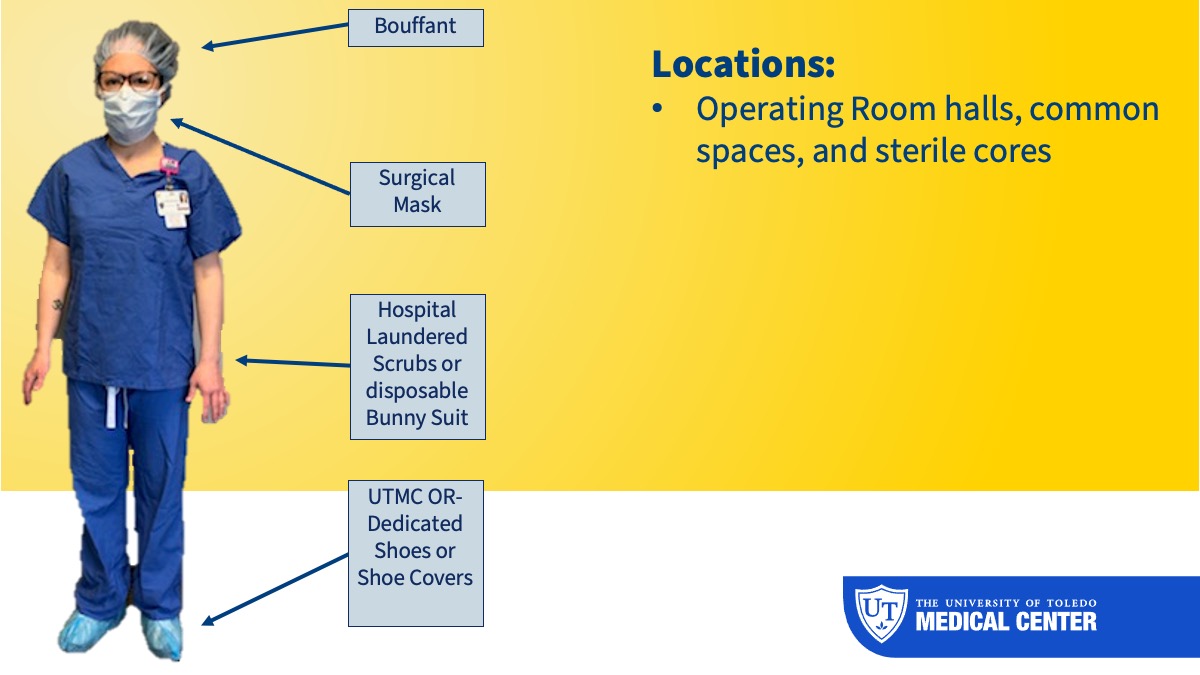
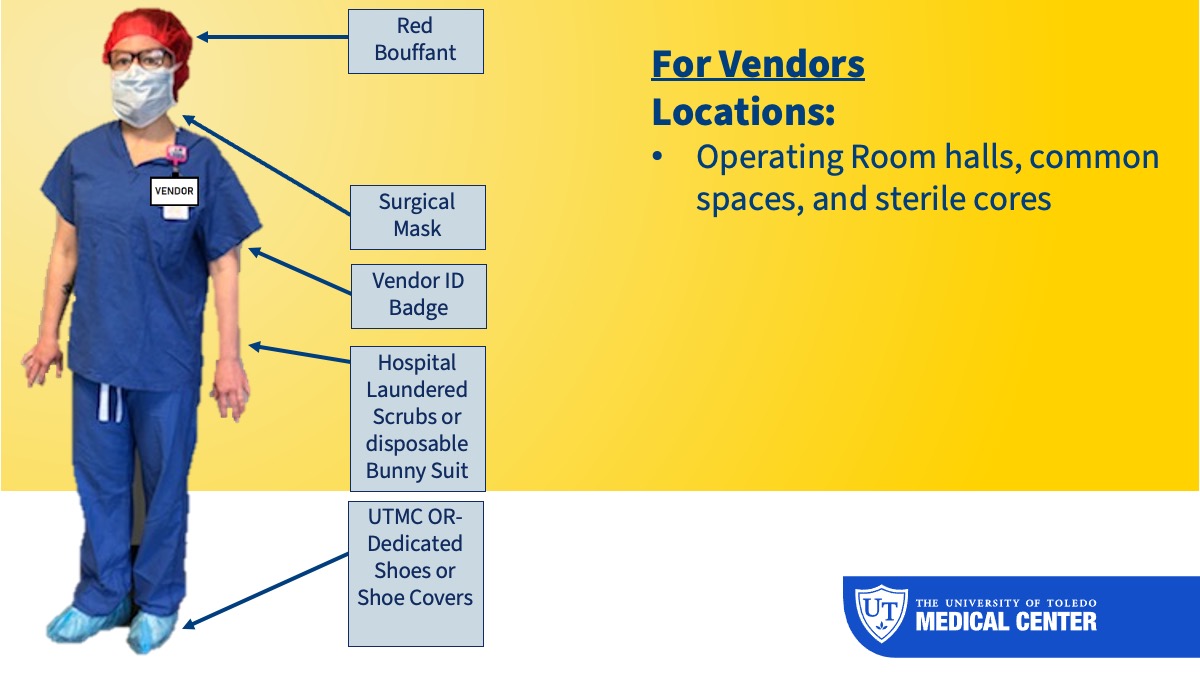
Updated Guidelines and Recommendations for the Operating Room
Attached, please find the Updated Guideline and Recommendations for the Operating Room, along with the Joint Commission position statement on preventing nosocomial infections.
Download the guidelines and recommendations (PDF)
Download the Joint Commission statement (PDF)
Signage from Nursing Administration
Any signage (floor stickers, social distancing signage and signs for the seating areas) for the clinical areas can be received from Nursing Administration.
What are we doing now at UTMC to help protect you?
At UTMC, we took proactive steps to ensure your safety. Here are some of these steps:
- Ensuring social distancing in public areas and in work and office environments
- Plastic barriers in place when social distancing is not able to be maintained
- Furniture removal and repositioning to assist with social distancing compliance
- Plexiglass barriers at registration areas and office spaces
- Face coverings for everyone that enters the university buildings, hospital, or clinics
- Disposable mask and eye protection to be worn by all staff while in clinical areas
- Increased cleaning frequencies for high traffic areas and frequently touched surfaces
- All patients are being tested for COVID-19 on admission, including SBH
- All surgical and procedural patients are being tested for COVID-19 at least 4 days prior to their scheduled procedure
- Increased hand hygiene stations placed throughout the facility including upon entry into the hospital
- Continued monitoring at entry points with temperature check in the hospital and clinics
- At the height of pandemic response, weekly updates to the Clinical COVID webpage https://www.utoledo.edu/coronavirus/clinical/
- Increased telemedicine office visits
- Contact tracing in collaboration with the local Health Dept.
- Established an outpatient healthcare testing clinic and a sick patient clinic for concerns of COVID-19
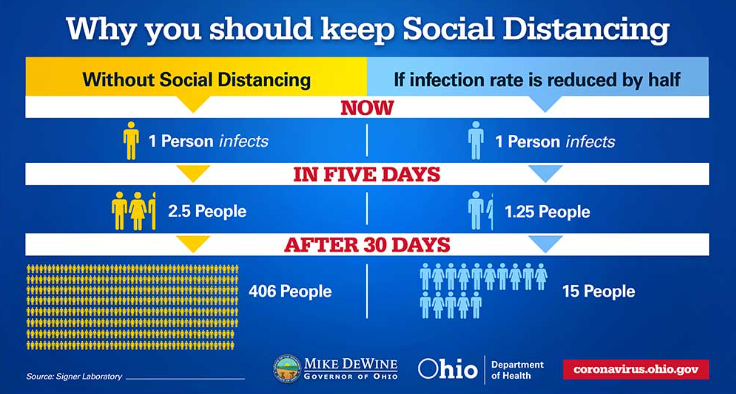
Social distancing: Why it’s important
As we have more individuals returning to work, social distancing must be a consideration and arrangements need to be made to accommodate the social distancing requirement. There will be additional direction, including resources (signage and floor markings) available over the next couple of weeks to assist with the reopening efforts.
RESTART Ohio
Stay current with the daily updates by visiting the RestartOhio Plan website.
Section Last Updated: Jan. 12, 2022, 5 p.m.
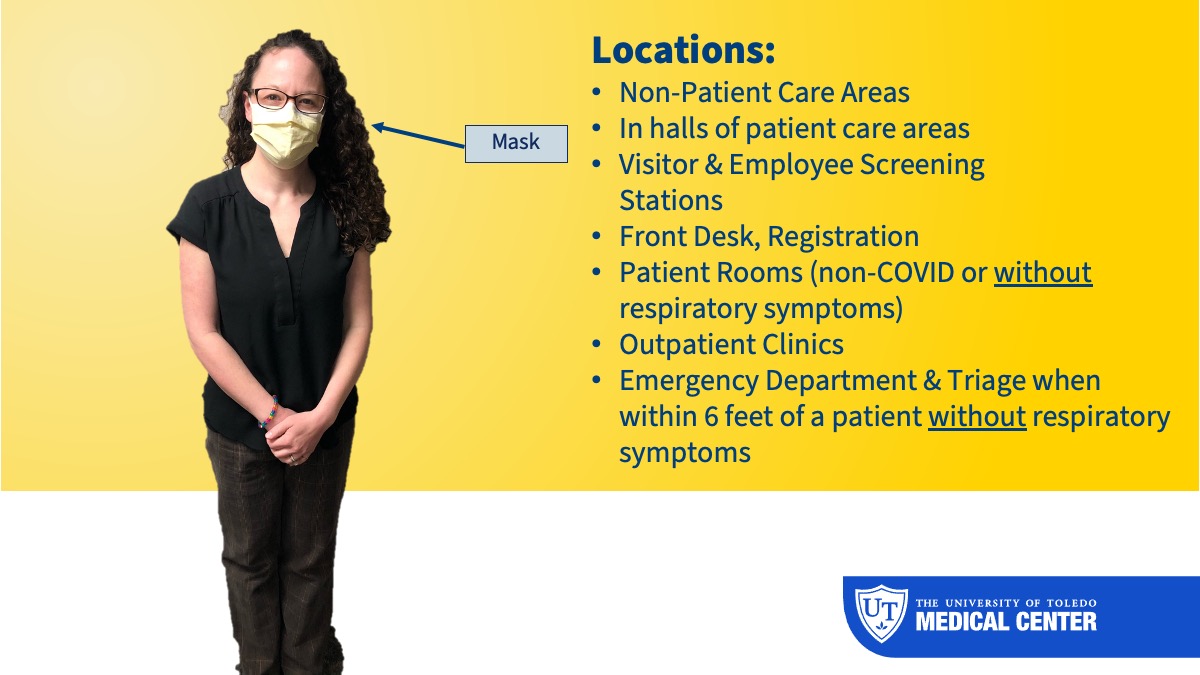
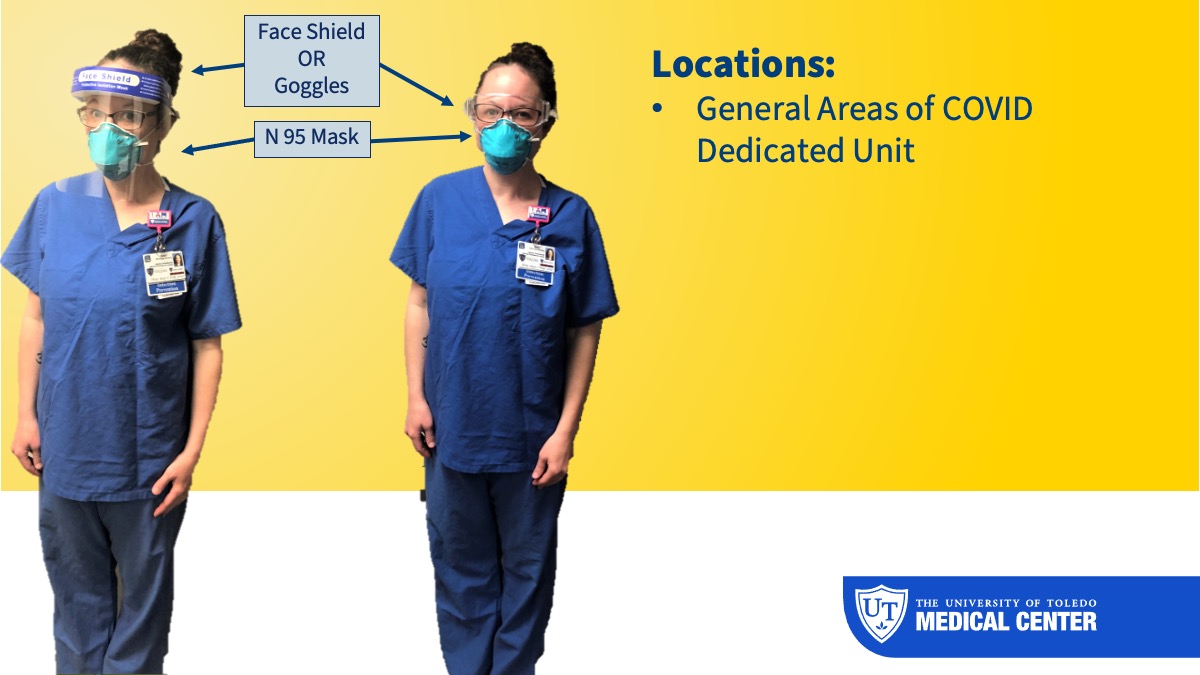
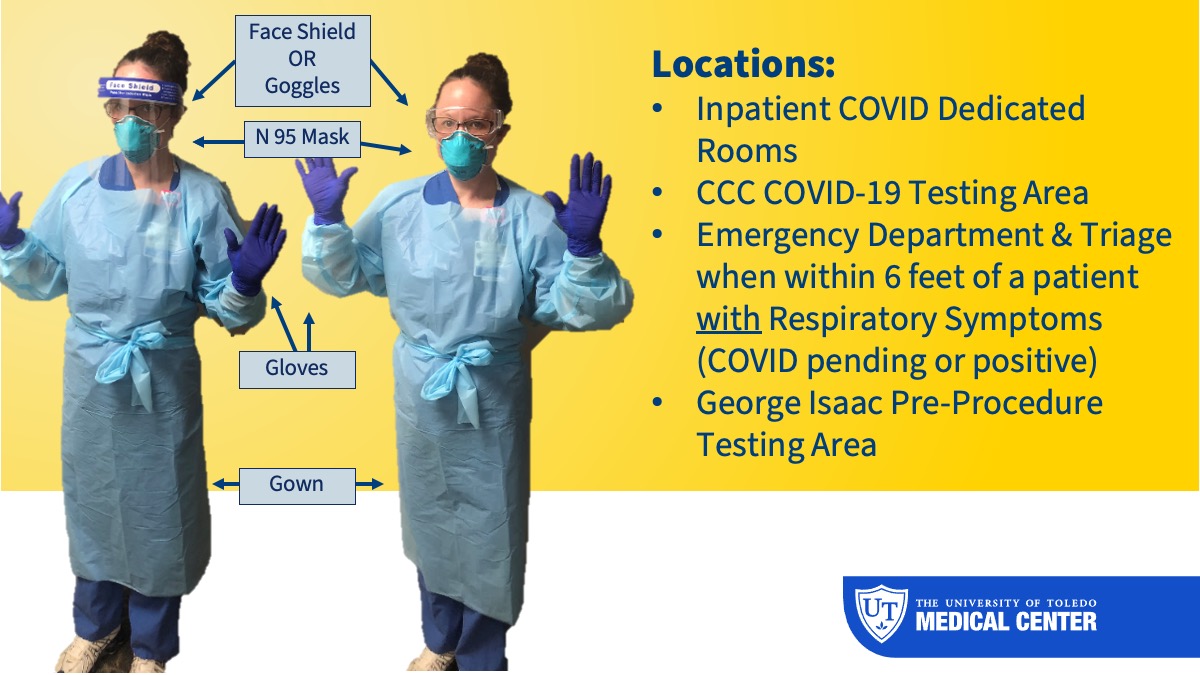
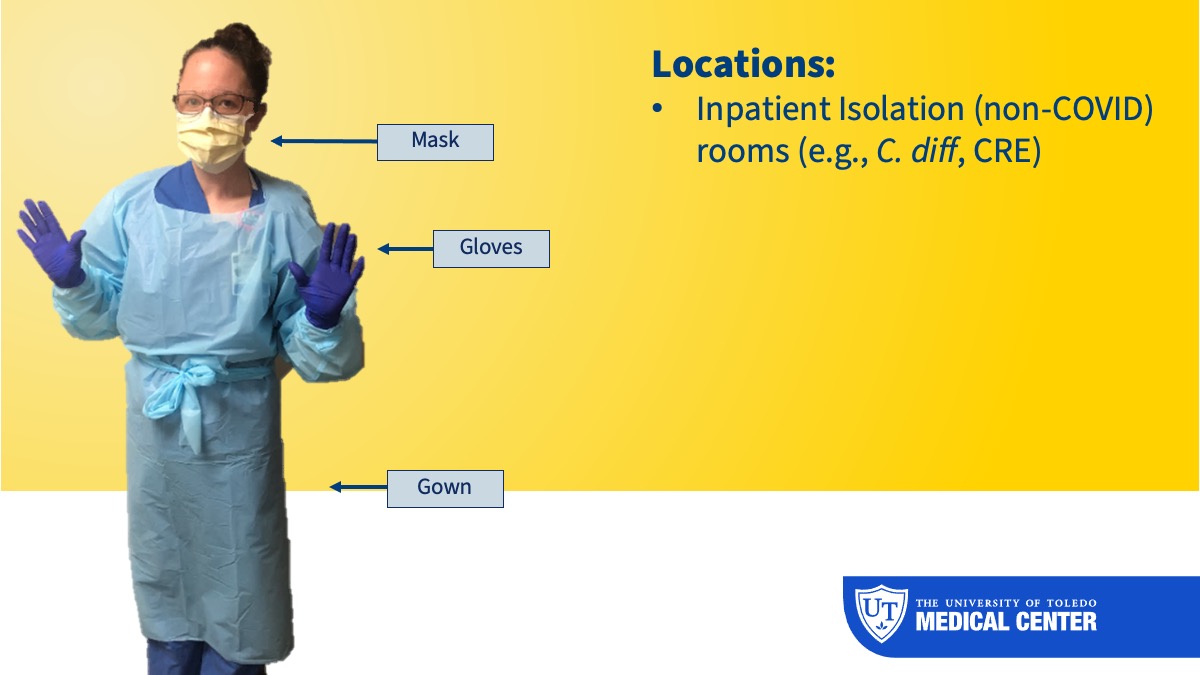
COVID-19 Personal Protective Equipment (PPE):
WHAT to wear and WHEN to wear it (Updated Jan. 10, 2022)
All University of Toledo personnel who report to work will wear a face mask (e.g., isolation or surgical mask).
If you are unclear about PPE requirements, or if you need access to required PPE, please talk with your direct supervisor to ensure you and those around you are properly protected.
See below the Updated Personal Protective Requirements, which includes the Operating Room and Vendors:
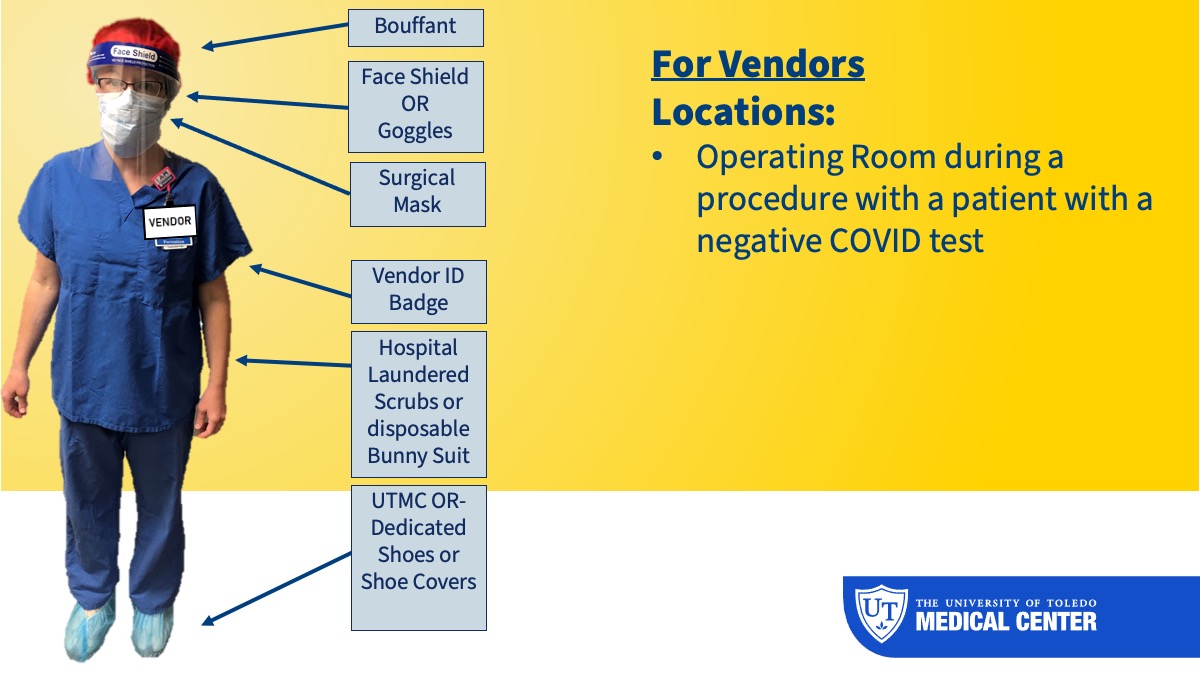
Download the updated, descriptive PDF
Visitor & Employee Screening Stations*
| PPE Type | All Areas |
| Gloves | Not required |
| Face mask | Required |
| Eye protection | Not required |
| Gown | Not required |
*All patients should have a non-cloth face mask upon entry into the hospital or clinic.
Front Desk, Registration*
| PPE Type | Front Desk Registration |
| Gloves | Not required |
| Face mask | Required |
| Eye protection | Not required |
| Gown | Not required |
*All patients should have a non-cloth face mask upon entry into the hospital or clinic.
Emergency Department, Including Triage*
| PPE Type | Patient Care with Respiratory Symptoms | Patient Care without Respiratory Symptoms |
| Gloves | Required† | Not required |
| Face Mask/N-95 or CAPR | N-95 or CAPR Required† | Face Mask Required |
| Eye protection | Required† | Not required |
| Gown | Required† | Not required |
*All patients should have a non-cloth face mask upon entry into the hospital or clinic.
George Isaac and Healthcare Provider Testing Area*
| PPE Type | COVID-19 Testing Area |
| Gloves | Required† |
| N-95 or PAPR | Required† |
| Eye protection | Required† |
| Gown | Required† |
*All patients should have a non-cloth face mask upon entry into the hospital or clinic.
†When caring for multiple COVID patients, you may enter a second COVID-19 patient
room without removing mask, eye protection, and gown, but must change gloves and sanitize
hands and patient care equipment between patient use.
Outpatient Clinic Areas*
| PPE Type | General Areas | Patient/Clinic Rooms |
| Gloves | Not required | Not required |
| Face mask | Required | Required |
| Eye protection | Not required | Not required |
| Gown | Not required | Not required |
*All patients should have a non-cloth face mask upon entry into the hospital.
Inpatient Non-COVID-19 Areas (MICU, 3AB, 4AB, 4CD, 5AB, 6AB, 6CD)*
| PPE Type | General Areas | Patient Rooms |
| Gloves | Not required | Not required |
| Face mask | Required | Required |
| Eye protection | Not required | Not required |
| Gown | Not required | Not required |
*All patient doors must remain closed.
COVID-19 Dedicated Rooms*
and Any Room with a COVID-19 Suspect or Positive Patient
(Limit staff to only those COVID-19 PPE trained from the following: RN, NA, Respiratory Therapy, EVS, Radiology, Pharmacy, and Physicians & APP)
| PPE Type | General Areas | Patient Rooms |
| Gloves | Not required | Required |
| N95 or CAPR | Not required | Required |
| Eye protection | Not required | Required |
| Gown | Not required | Required |
*All patient doors must remain closed.
**Once a patient is suspected or confirmed COVID positive, fit tested N95 or PAPR must be worn in patient room.
Additional information
Patient Placement
- Place appropriate precautions sign outside door.
- Airborne Infection Isolation Rooms (AIIRs) should be reserved for patients who will be undergoing aerosol-generating procedures as they are available.
- Ensure facilities is contacted to be made aware of the negative pressure room being utilized.
PPE Reminders
- Reuse N95 mask until it becomes visibly soiled, saturated, bent, broken, or you are unable to breathe through it.
- The mask should cover your mouth, nose and chin.
- The mask should not be pulled down and worn under your chin to expose your mouth and nose. This could place you at risk for contaminating yourself.
- Avoid touching the front of the mask unless you just performed hand hygiene.
- Wash hands before and after applying or removing mask.
- Reuse CAPR and disinfect per instructional video for reuse until broken or torn.
- Hold each other accountable to wear PPE correctly and safely.
Limit exposure
- Exclude all healthcare workers not directly involved in patient care from entering COVID-19 designated room(s), when suspected or confirmed COVID-19 patient is present.
Trash & Linen
Management of laundry, food service, and medical waste should be performed in accordance with routine procedures.
Dietary Trays
- In designated COVID-19 room(s) and area(s), Food and Nutrition Services to notify nursing staff upon delivery of dietary tray & wait outside for staff to obtain tray.
- Disposable portion of the tray to be delivered to the room by the nurse.
Phlebotomy & Specimen handling (Nursing & Lab)
- Staff entering the patient room must don & doff appropriate PPE.
- Specimen collection bags: With clean gloves, use inside out method with second bag to grab specimen OR double bag the specimen using a clean staff member at the room door when available.
Diagnostics/ Equipment
- Perform all necessary procedures and tests in the patient room whenever possible.
- Clean and disinfect all equipment after used in patient room with approved product.
Rapid Response/Code Blue
- Don appropriate PPE prior to entering isolation room.
- Limit entrance to room to those directly involved in patient care.
Students/Learners
- No students or learners to enter COVID-19 isolation rooms.
- For attending providers, learner may enter the room while with the attending.
Transport
For ALL suspected or confirmed COVID-19 patients:
- Place a mask on the patient.
- If they are on a ventilator, do not place a mask. Respiratory Therapist will apply a filter to the exhaust port of ventilator.
- Place a clean flat sheet over the entire bed up to the patient’s neck.
- Prior to entering the room, don gown, gloves, masks, and eye protection.
- Doff gloves and gown after assisting patient to transport bed or chair but prior to leaving room.
- Patient to be transported to the testing area using clean gloves and N-95 or CAPR/PAPR.
- Wait in appropriate designated area during testing.
- Patient to be transported back to patient room using clean gloves and N-95 or CAPR/PAPR.
- Prior to entering the room Don gown, gloves, masks, and eye protection.
Aerosol-Generating Procedure
Aerosol-generating procedures include: Intubation (during intubation), extubation, BiPAP, high flow oxygen, open suctioning, sputum induction, bronchoscopy, aerosol treatment, nasopharyngeal or oropharyngeal specimen collection.
Room door to remain closed, and patient in negative Airborne Infection Isolation Room (AIIR) if available.
These require clinician to wear the following PPE:
- Fit tested N95 and eye protection or CAPR/PAPR
- Gloves
- Gown
Download the complete PDF (Jan. 10, 2022)
Update (Oct. 11, 2021)
Currently, UTMC has a good stock of N-95 and our Supply Chain Dept. noted that they
do not have any supply issues with N-95s at this time. Because of this, we wanted
to update you on N-95 mask use to help with the work flow as best as possible yet
maintain safety and limit exposure to COVID-19:
- Please wear a procedural/isolation mask over your N-95 and change the procedure mask
in-between each COVID-19 patient
- Discard the N-95 if it becomes contaminated with blood, respiratory or nasal secretions, or other bodily fluids from patients
- Please wear eye protection or a face shield (as long as the shield does not compromise
the N-95) while in COVID-19 patient rooms or in rooms with a patient that has a respiratory
illness
- The N-95 should be discarded prior to leaving the unit or before you go into a non-COVID-19 patient room
- Once the N-95 is removed, discard it
- When it is required again, replace it with a new unused N-95
A note about face shields
A face shield does not fully cover the mouth to prevent the spread of the virus. If someone wearing a face shield were to cough
or sneeze, particles could still exit on the bottom of the face shield. The hospital
isolation masks can be provided to these patients if they come in a face shield.
Here is the link to the CDC’s guide to masks which will help provide more information.
Face Covering Requirements and Guidance (Oct. 9, 2020)
Face coverings are required for employees at all times unless in an enclosed office space with the door closed. Cubicles with an open top are not considered an enclosed space and face coverings must be worn while in this space per Ohio Dept. of Health.
Ohio Requirements (May 8, 2020)
In line with guidance from the Ohio Governor, Mike DeWine, The University of Toledo is now requiring that all employees in non-clinical areas wear cloth face coverings to help reduce the spread of COVID-19.
Disinfecting Procedure for Mobile Tablets (April 24)
Mobile tablets are becoming more popular in the healthcare environment; however, they may carry nosocomial pathogens due to the various ports and crevasses. To ensure that appropriate cleaning is performed as required to aid in preventing the transmission of infection, and to ensure actions are taken to keep equipment maintained in optimal functionality and cleanliness, please follow the following procedure:
Reminder about cloth masks
Cloth masks are non-medical, are not considered PPE but an alternate to PPE and should not be worn in patient care.
Approved COVID cleaning chemical list
See the list of COVID-19-approved products, updated Aug. 25, 2021.
How is Coronavirus Disease 2019 (COVID-19) spread?
COVID-19 spreads when an infected person breathes out droplets and very small particles that contain the virus. These droplets and particles can be breathed in by other people or land on their eyes, noses, or mouth. In some circumstances, they may contaminate surfaces they touch. People who are closer than 6 feet from the infected person are most likely to get infected.
COVID-19 is spread in three main ways:
- Breathing in air when close to an infected person who is exhaling small droplets and particles that contain the virus.
- Having these small droplets and particles that contain virus land on the eyes, nose, or mouth, especially through splashes and sprays like a cough or sneeze.
- Touching eyes, nose, or mouth with hands that have the virus on them.
For more information about how COVID-19 spreads, visit the How COVID-19 Spreads page to learn how COVID-19 spreads and how to protect yourself.
Healthcare workers (HCW) have increased risk of exposure to SARS-CoV-2, the etiologic agent of COVID-19. The CDC is currently recommending the following strategies to mitigate exposure and risk.
The difference between Surgical Masks and N-95 Respirators
Videos
Videos have been created for how to put on and take off Personal Protective Equipment (PPE) as well as daily room cleaning instructions for nursing staff. Those videos have been uploaded and assigned for staff on the UToledo Test Bank.
Section Last Updated: May 27, 2022, 3 p.m.
UTMC Guidance for COVID-19 Management
The treatment guidance for COVID-19 was updated on June 30, 2022.
- If there is a non-urgent, non-surgical procedure (e.g., EGD, TEE) and the patient test is positive for COVID-19:
- For symptomatic cases:
- Procedure can occur after 10 full days from symptom onset with the first day of symptoms being day “0,” as long as their symptoms have improved and they are without a fever for 24 hours
- For asymptomatic cases that have not been previously positive in the preceding 90 days:
- Procedure can occur after 10 full days of positive test with day of test being day “0”
- If the patient develops symptoms during this time period then the “For symptomatic cases” process should be followed
Treatment Update (May 18, 2022)
Paxlovid (if clinically appropriate) is the agent of choice for outpatients with mild to moderate COVID-19 with certain risk factors according to the NIH and UTMC guidelines. If the use of Paxlovid is not feasible or appropriate, bebtelovimab (monoclonal antibody injection) or molnupiravir (oral capsules) are alternative options; however, these agents lack strong clinical efficacy data to support their routine use. Please refer to the UTMC COVID-19 Guidelines for additional information.
Monoclonal Antibodies
Available Agents
- Bebtelovimab
- Bebtelovimab Paper Order (Updated April 12, 2022)
- Link to Download Patient/Caregiver Fact Sheet
- Cilgavimab/tixagevimab
- Cilgavimab/tixagevimab Paper Order (Updated June 30, 2022)
- Link To Download Patient/Caregiver Fact Sheet
Process for Ordering Monoclonal Antibodies:
With Infectious Diseases approval, inpatient orders (for patients with non-COVID-19 primary diagnoses) should be faxed to Central Pharmacy at 419-383-2828.
Please check with the coordinating staff at 419.383.4432 to see what is in stock before submitting orders.
- Fax order to UTMC BOP room 419.383.3371:
- BOP room will coordinate registration and scheduling of the patient at UTMC
- Call 419.383.4545, Option 4 to schedule treatment for Monoclonal antibodies
- Your call will be returned the same business day for scheduling
- Prescriber must discuss with the patient this is not an FDA-approved medication
- Prescriber must document in the medical record the EUA sheet was discussed and that a copy of the EUA was provided to the patient for review
- Prescriber must also document in the medical record (Athena or ED note in McKesson) the patient verbally consented to the treatment
Process For Ordering INPATIENT Monoclonal Antibodies If They Are Eligible:
- Primary admission diagnosis must be another reason other than COVID-19
- Requires Infectious Disease Physician approval
- Order form to be faxed to the pharmacy at 419.383.2828
- Prescriber must discuss with the patient this is not an FDA-approved medication
- Prescriber must document in the medical record the EUA sheet was discussed and that a copy of the EUA was provided to the patient for review
- Prescriber must also document in the medical record the patient verbally consented to the treatment
CDC Health Advisory (Aug. 26, 2021): Rapid Increase in Ivermectin Prescriptions and Reports of Severe Illness Associated with Use of Products Containing Ivermectin to Prevent or Treat COVID-19
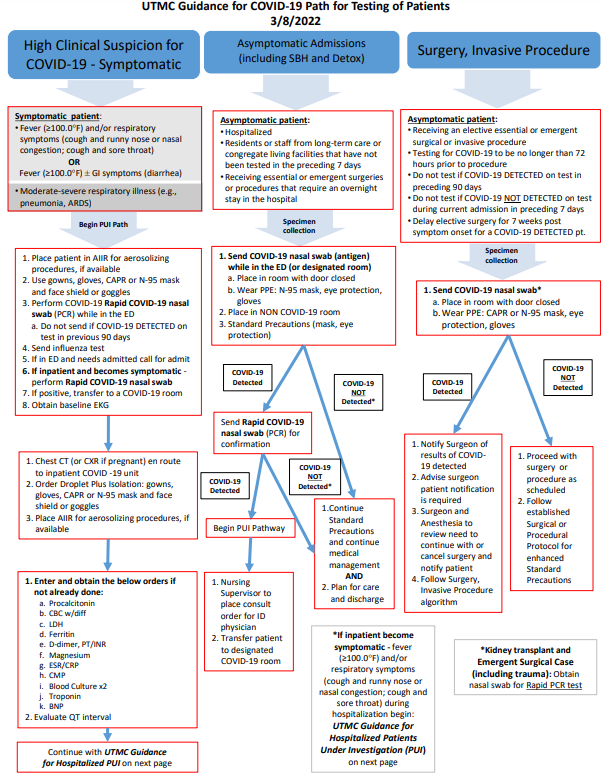
Updated Testing Pathway (March 8, 2022)
Please review the below updated pathway:
COVID-19 screening tool
Download the COVID-19 Screening Tool.
Clinical diagnosis:
Currently, the diagnosis of COVID-19 should be suspected in the following settings:
- Patients with fever and symptoms of lower respiratory tract infection who have had
prolonged, close contact (within 6 feet) with a confirmed or suspected COVID-19 patient,
as defined by the CDC as:
- Being within approximately 6 feet (2 meters) of a COVID-19 case for a prolonged period
of time; close contact can occur while caring for, living with, visiting, or sharing
a health care waiting area or room with a COVID-19 case.
- OR - - Having direct contact with infectious secretions of a COVID-19 case (e.g., being coughed on).
- Being within approximately 6 feet (2 meters) of a COVID-19 case for a prolonged period
of time; close contact can occur while caring for, living with, visiting, or sharing
a health care waiting area or room with a COVID-19 case.
- Patients with severe lower respiratory tract disease when an alternative etiology cannot be found
Once local/community transmission has been reported in a geographic area, the all patients with symptoms of acute respiratory illness should be considered as suspected cases.
Laboratory/radiology findings:
The following lab findings can be seen in COVID -19:
- Leukopenia, lymphopenia, elevated LFTs
- But leukocytosis can be seen in up to 30% of patients
- Normal procalcitonin in absence of secondary infection
- CT scans with bilateral ground glass opacities
- Usually peripheral
- Usually involving the lower lobes
- May also see effusions and lymphadenopathy (less commonly)
PCR, Culture, and Antibody Testing
- Viral culture of suspected cases is discouraged except in the research setting
- Antibody testing (IgG/IgM) is not readily available in the U.S. at this time but that will be coming soon
- Currently, rtPCR of nasopharyngeal specimens is the main mechanism for confirmation
of suspected cases
- Long waiting time for results
- Sensitivity may be as low as 60%
Diagnosis
Download the UToledo Adult Order Set - April 15, 2020 (PDF)
Section Last Updated: Jan. 25, 2022, 5 p.m.
Isolation Decision Algorithm (Jan. 20, 2022)
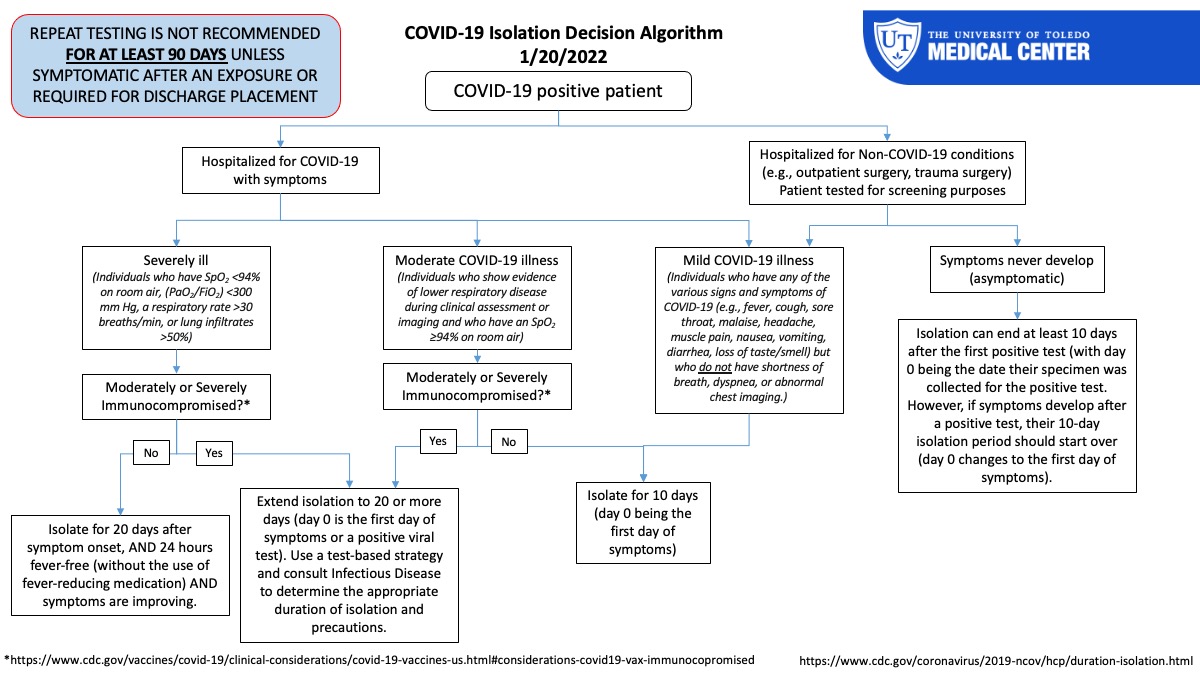
Plan for Admitted Patients
Learn more about the plan for COVID-19 positive/High Clinical Suspicion admissions at UTMC, effective June 8, 2021.
Patient presenting to the ED requiring admission:
See Emergency Department Guidance (PDF) for patients who require admission with respiratory Illness Suspected COVID-19.
By the Numbers
TOTAL= 121
Section Last Updated: Dec. 16, 2021, 3 p.m.
UTMC Discharge Instructions
Download the following PDF instructions:
Discharge for confirmed COVID-19 patient - Dec. 2021
Discharge for patient tested for COVID-19 (awaiting test results) - Dec. 4, 2020
Previous Documents:
Discharge for Confirmed COVID-19 Patients - Aug. 20, 2021
Discharge for patient suspected of COVID-19 (testing not performed) - May 29, 2020
Section Last Updated: Oct. 9, 2020, 12 p.m.
Q: Can SARS-CoV-2, the virus that causes COVID-19, be transmitted by blood transfusion?
A: In general, respiratory viruses are not known to be transmitted by blood transfusion,
and there have been no reported cases of transfusion-transmitted coronavirus.
Visit the FDA’s Frequently Asked Questions page
Our understanding of COVID-19, the disease caused by the novel coronavirus SARS-CoV-2, is rapidly evolving. Here are some important things to know:
Incubation period:
2 – 14 days (median 4-5 days)
Transmission:
Droplet (information about fomites and fecal-oral routes of spread are evolving)
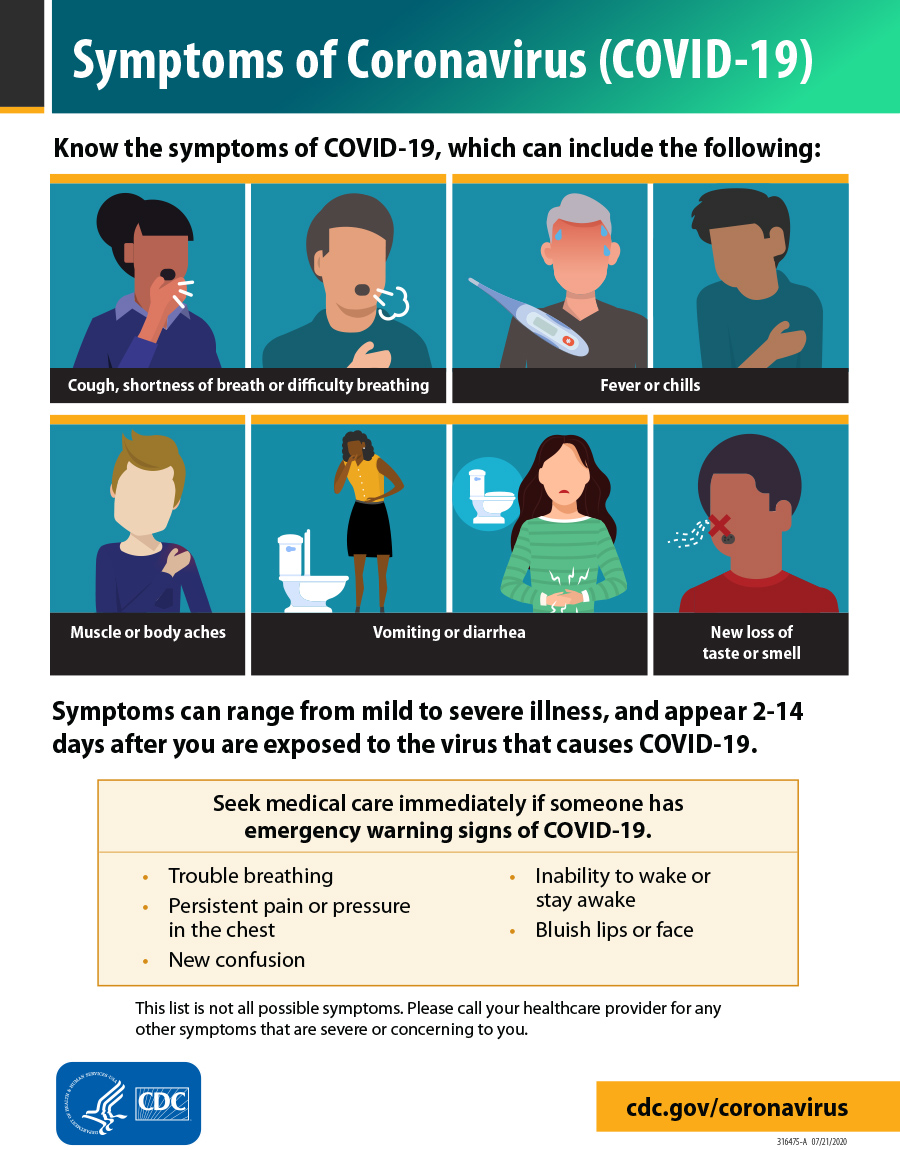
Clinical manifestations:
- Range of illness seen
- 80% asymptomatic/mild to moderate
- 15% severe (defined as shortness of breath, hypoxia, >50% lung involvement)
- 5% critical (defined as respiratory failure, shock, multi-organ system failure)
- 2.5% mortality rate among the critically ill
- ARDS, arrthymias, ARF commonly seen
- 2.5% mortality rate among the critically ill
- Key clinical findings
- Fever (majority of patients)
- May be prolonged and intermittant
- Dry cough (sputum production or hemoptysis less common)
- Shortness of breath/chest discomfort
- Flu-like symptoms (fatigue, myalgias, headache)
- New loss of taste and smell
- GI symptoms
- URI symptoms such as sore throat, congestion or runny nose
- Fever (majority of patients)
- Key features of clinical course
- Significant clinical change/deterioration has been described after the first week
of illness
- Significant complications such as ARDS have been reported an average of 8 days after symptom onset
- Significant clinical change/deterioration has been described after the first week
of illness
For more information, visit the CDC website on COVID-19 clinical guidance
Section Last Updated: Aug. 17, 2021, 2 p.m.
It is normal to feel some degree of anxiety or concern and even exhaustion as we progress through this pandemic. But, above all, we need to remain calm and take care of ourselves and loved ones. In addition to good hand hygiene, cleaning & disinfecting, getting vaccinated, maintaining social distancing and properly wearing a mask/face covering, here are some important steps we might not think about to keep everyone healthy.
- Be informed with factual information. This will help you keep things in perspective and not inflate the risk. Know real
facts from reputable sources and, evaluate your own personal risk and that of your
family members according to factual information. Sites such as the CDC are kept constantly
up-to-date.
- Take action. Make informed preparations and take realistic precautions. As they say, “knowledge
is power” and having confidence that you know the right things to do to protect yourself
and your family is important to controlling your anxiety and preventing illness.
- Do not overload on media. Staying updated is a good thing, but too much of anything, including new reports,
can have a negative effect and can increase your feeling of immediate threat and vulnerability.
It can trigger your “fight or flight” response to a threat. Watching non-stop news
about the spread of the virus is not conducive to good mental health. So, limit your
media exposure about the virus.
- Keep yourself physically healthy. Eat healthy foods, go outside, get yourself and your family moving with physical
exercise and get a healthy amount of sleep. Giving into exhaustion and sitting in
your favorite chair all evening, binging on junk food, smoking more, or increasing
your alcohol consumption may be some of the ways we have coped in the past, but, are
not in the category of good health practices! Use this opportunity to re-evaluate
some of your health practices and, if necessary, make some needed changes!
- Keep yourself mentally healthy. Think about ways you have dealt with anxiety and exhaustion in the past and be open to exploring some new strategies. For example, you might talk to a friend or family member, use yoga or meditation, read a book, watch an uplifting movie, get some exercise or work in your garden on nice days. A number of resources can be found on the ADAA website. You might find one of these apps helpful:
- Simple Habit
- Breathe & RelaxCalm
- Insight Timer
- Have (and be) a support network. Maintain contact with family, friends and co-workers. Reach out. Keep in touch with
and check on people who are particularly at risk or isolated and alone help them stay
connected and supported. Using FaceTime, Skype, and/or other similar video apps can
help.
- Keep a routine. With disruptions in our schedules, cancellations and other “social distancing measures,”
it can be easy to fall at loose ends. Establish a new routine for yourself and/or
your family, switch things up periodically with a new routine. Whatever you do, it
is important that you establish a “new normal”, even in the midst of disruption in
our usual schedules and usual life styles.
- Get some help if you need it. Sometimes, it can be helpful just to have someone to talk to about our concerns and anxieties. Some people who have a history of mental health issues or who are already feeling overwhelmed by life challenges may find their anxiety and/or depression heightened during a stressful period such as this.
If you feel it would be helpful to talk to someone, here are some resources:
- UToledo/UTMC Faculty & Staff can call a 24-hour helpline at IMPACT: 800.227.6007
- UTMC Outpatient Behavioral Services: 419.383.5695
- UToledo students can call the University Counseling Center that also has a 24/7 helpline number: 419.530.2426
Wellness resources
If you are experiencing increased anxiety or stress related to concerns about COVID-19,
you may benefit from seeking counseling.
Faculty and staff should contact their mental health provider or reach out to the
University’s Employee Assistance Program (EAP) or call 1-800-227-6007 (Use “UT” as the username).
Section Last Updated: Jan. 5, 2022, 2 p.m.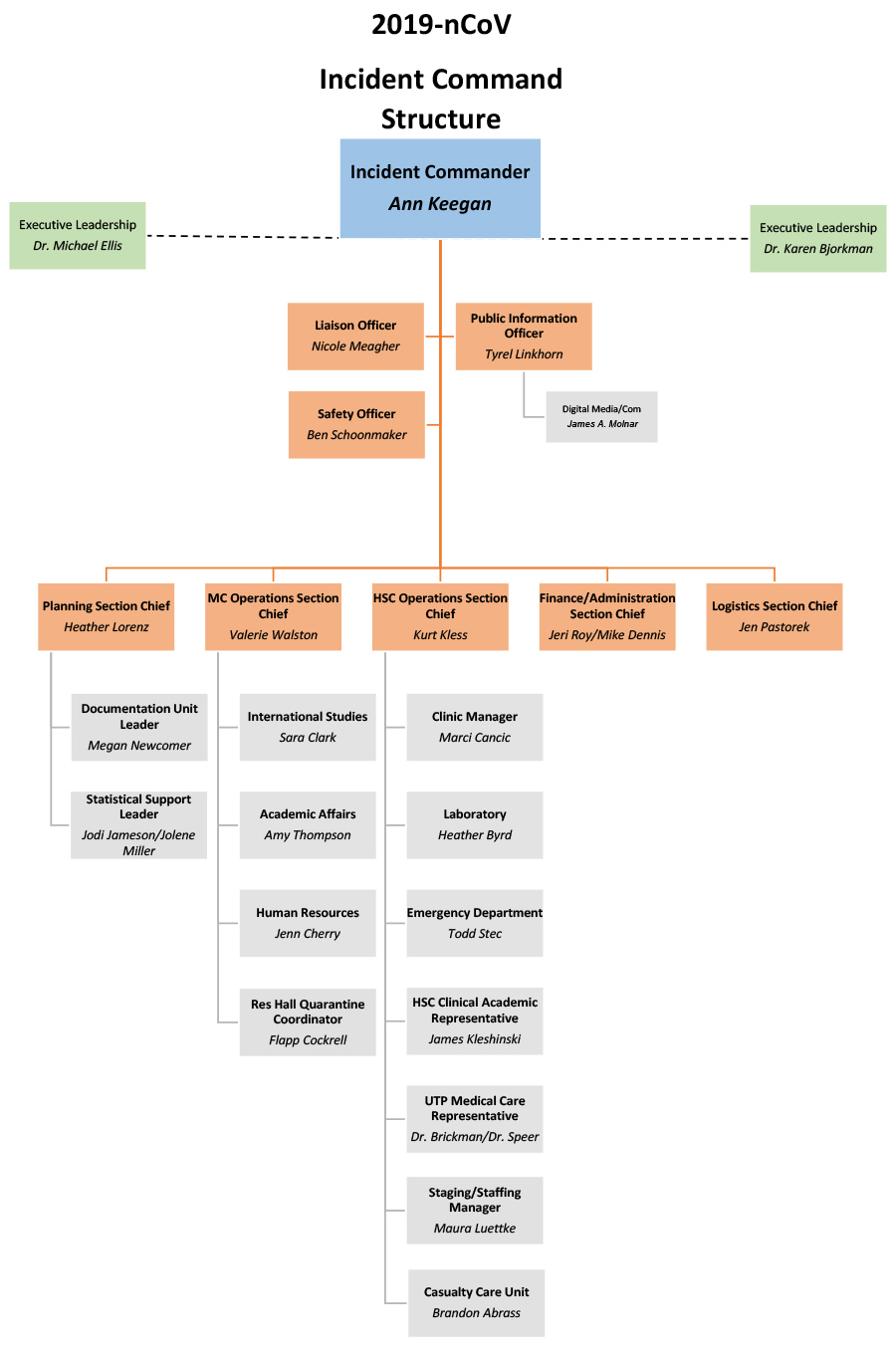 As the COVID-19 pandemic became a reality for our community and institution, our Incident
Command System (ICS) was implemented early in the Pandemic. The COVID-19 Incident
Command team began planning and preparing to implement strategic plans to effectively
deal with the COVID-19 crisis. One look around our institution and people can see
the many changes that took place, due to the efforts of the ICS. The visible changes
that were implemented only represent a small part of the overall COVID-19 preparedness and
response efforts.
As the COVID-19 pandemic became a reality for our community and institution, our Incident
Command System (ICS) was implemented early in the Pandemic. The COVID-19 Incident
Command team began planning and preparing to implement strategic plans to effectively
deal with the COVID-19 crisis. One look around our institution and people can see
the many changes that took place, due to the efforts of the ICS. The visible changes
that were implemented only represent a small part of the overall COVID-19 preparedness and
response efforts.
Currently, the full ICS is inactivated, however if need arises, select sections in
the ICS will be activated to respond accordingly. We continue working in close cooperation
with the Ohio Department of Health, the Toledo-Lucas County Health Department, and
our regional partners in healthcare in Northwest Ohio.
The Pandemic continues to be fluid situation. And as the situation changes, we will
need to rapidly respond. But we are committed to keeping you informed of these changes
and keeping you safe. This webpage provides you with up-to-date information to help
protect you, and help you do your job.
The Incident Command System (ICS) (as seen above in the chart) is a standardized approach to the command, control, and coordination of emergency response. It is important that we streamline questions and concerns through the appropriate chain of command. When the ICS is operational, all logistical concerns, including supplies and donations, would go through the Logistics Section Chief. All clinical operation questions would go through the appropriate unit leader who will report up through the Clinical Operations Section Chief. Infectious Disease questions would be directed to the Medical Technical Specialist. When operational, all questions would then be addressed at the daily incident command meeting. Learn more about ICS from FEMA.
Questions and Comments
Please note, we recommend you read the full webpage before submitting any questions or comments. What you submit will be directed to the appropriate party and they will follow-up accordingly.
Hotlines
- ODH Informational hotline: 833-4ASK-ODH
- Support hotline: If you are feeling so overwhelmed that you’re having thoughts of harming yourself, please know that there are safe places to call including 1-800-273-TALK (8255).
Section Last Updated: Aug. 17, 2021, 2 p.m.
Caring for COVID-19 patients
The University allows residents and fellows to participate in the care of COVID-19
patients. All residents are required to watch the PPE training video. To participate, they must undergo training for mid-level PPE. This is in accord
with our directive that “only residents and fellows who have completed the mandatory
COVID-19 educational session will be allowed to participate in direct patient care
with suspected or proven COVID 19 patients.”
We also remind everyone that participation requires:
- Minimal contact: Direct care provided by any resident or fellow should involve the fewest number
of trainees and the least amount of time spent in direct contact with the COVID-19
patient. In most, if not all cases this will mean 1 resident or 1 fellow, and
- Adequate supervision: Residents and fellows providing care to COVID-19 patients will do so under the appropriate
supervision for the clinical circumstance and the level of education of the resident/fellow.
- Adequate Training (see above)
Daily Symptom Monitoring (May 1, 2020)
Daily symptom monitoring means people should monitor their temperature daily (anything
greater than 100.0°F / 37.8°C) before the start of their shift and remain alert for
respiratory symptoms (e.g., fever and/or respiratory symptoms – cough and runny nose
or nasal congestion; cough and sore throat). If symptoms develop, one should self-isolate.
Self-isolation recommendations: stay in another room or be separated from others,
using separate bedroom and bathroom if available.
**Employees will no longer need to report their temperature in the employee temperature self-monitoring application.
The best way to prevent illness is to avoid being exposed to this virus:
- Practice social distancing.
- Avoid close contact with people who are sick.
- Avoid touching your eyes, nose, and mouth.
- Stay home when you are sick.
- Cover your cough or sneeze with a tissue, then throw the tissue in the trash and wash your hands.
- Clean and disinfect frequently touched objects and surfaces using a regular household cleaning spray or wipe.
- CDC recommends wearing cloth face coverings in public settings where other social distancing measures are difficult to maintain (e.g., grocery stores and pharmacies), especially in areas of significant community-based transmission.
Section Last Updated: April 13, 2020, 4:00 p.m.
Section Last Updated: April 6, 2020, 8 p.m.
Containment vs. mitigation
We have learned from our epidemiology and infectious disease colleagues the ways that
these events are handled change as the situation changes. Early the strategy is “containment.” We
aggressively quarantine people that have been to high-risk areas. As an example, someone
who traveled to Wuhan, China. However, once community-wide spread occurs, it may
become impossible to quarantine all healthcare workers, thus the strategy moves to
mitigation. With mitigation, healthcare workers will be allowed to work, as long as
they don’t have symptoms or signs (a temperature over 100 degrees) of infection. Employees
caring for patients under investigation or with known COVID-19 can continue to work
as long as proper PPE is being worn at all points of care. Thus, it is critically
important that we reduce healthcare worker exposure with appropriate use of PPE and
pay attention to social distancing at home and at work.
Ambulatory
Section Last Updated: April 30, 2020, 4 p.m.
UTMC
Section Last Updated: Aug. 7, 2020, 12 p.m.
Newsletter Archive
COVID-19 At-a-Glance
Statistics
We are sharing the updated COVID-19 stats, clinical trial information and literature via a new page on the UToledo Libraries COVID-19 Library Guide (to print easily from this page, scroll down to the bottom and click on "Print Page").
View statistics via UToledo LibGuides
News
from the Literature
Below are selected highlights from the recent literature. For a real-time, updated
list of the latest articles in PubMed,
see the University Libraries COVID-19 LibGuide
Keeping up with COVID-19 Literature View all previous selections from the literature
Clinical Trials
clinical trials related to COVID-19
Updates from Ohio Governor Mike DeWine
COVID-19 Update:
- Governor DeWine Encourages Student Athletes to Get Vaccinated (6/18/21)
- State of Emergency to be Lifted, Vax-A-Million Winners (6/17/21)
Visit the State of Ohio Coronavirus website
Data Sources
- Centers for Disease Control and Prevention: COVID-19 Cases in U.S.
- Johns Hopkins University Center for Systems Science and Engineering: COVID-19 Global Cases Map.
- Michigan Department of Health and Human Services: COVID-19 (Daily Confirmed Cases and Cumulative Data)
- Ohio Department of Health: COVID-19
- Toledo-Lucas County Health Department: Coronavirus Information
- World Health Organization: COVID-19, Situation Dashboard
- World Health Organization: COVID-19, Situation Reports
For More Information
Mulford Reference Assistance: MulfordReference@utoledo.edu or 419.383.4218 (please leave a voicemail)
Jodi Jameson, Nursing Librarian, jodi.jameson@utoledo.edu or 419.383.5152